Telehealth is gaining momentum in the domain of healthcare technologies. 91% healthcare professionals use telemedicine, offering one or more types of this service. New applications emerge daily to improve patient outcomes, ensure better patient experience, enhance patient information security, and provide medical businesses with a competitive advantage. Unfortunately, organizations often make faults with diagnostic accuracy, customizability, UX/UI design, scaling software and protecting PHI while launching telemedicine software, which does not allow them to benefit from such solutions.
In this material, we will describe the most common challenges that telemedicine software development company experience and explain how to solve them.
Common challenges in telehealth platform implementation
The healthcare systems are notoriously resistant to any kind of reforms. And it’s not the software development that complicates the adoption or revamping, it’s the regulation. Telehealth platforms are quite unflexible due to compliance requirements, licenses, and numerous regulations.
Strong compliance
It might be challenging to provide clinical data by governmental guidelines. Patients fear that someone may hack or sell their medical information. There’s always a slim chance that a hospital, health system, healthcare software supplier, or practice might go out of compliance with just one error, which could result in substantial fines.
Parity payments
When it comes to telemedicine, parity implies that insurance companies should generally pay around the same amount whether you receive care in person or via Zoom. Because they would otherwise not get paid, many doctors now request that the patient come into the office. Even though many providers gradually include a few telehealth services in their reimbursement rates, not all patients can access these services due to industry resistance.
Multi-state licensure
Despite all growing acceptance rates, 21 states continue to prohibit the practice of medicine outside of their boundaries, ostensibly to protect their local license holders. Therefore, a provider who holds a California license cannot offer services in Idaho. However, we occasionally observe legislative action that aims to permit interstate telemedicine.
Slower adoption
Due to limited IT funds, outdated systems, and a labor shortage, hospitals have been sluggish in implementing telemedicine technology in most countries. Today's telemedicine, nevertheless, is managed by startups, such as MDLIVE in the US, Babylon Health in the UK, and Doktor24 in Sweden. These companies, however, have had a difficult time up until now getting past reluctance from traditional healthcare institutions.
In some respects, it feels like we've moved into the future since telehealth has been accepted quickly and extensively in ways that no one could have imagined six months ago, enabling access to treatment that would not have been possible otherwise. Despite all this, telemedicine is still developing, and more and more solutions such as how to build a telemedicine platform. are being implemented yearly.
Create, renovate, and expand your telehealth solutions with us
7 Barriers to telehealth software adoption
The main barriers and limits associated with telehealth adoption are its security and privacy concerns. Anyone, including unauthorized users, can use the software. This could lead to data breaches and loss of patient information. Additionally, telehealth faces boundaries with its cost and scalability. While it is reasonably priced, it may not be accessible to all patients. Let’s dig more into barriers to find out in detail.
1. Avoiding excessive expenses
The launch of a telehealth app that provides a broad range of functionalities and ensures high quality is inevitably associated with significant expenses. A recent report has revealed that developing a mobile telemedical application may cost healthcare providers up to $425,000 .
One of the main reasons leading to such immense expenses is that healthcare providers frequently lack the technical expertise required for choosing the most cost-efficient solutions. Limited technical knowledge is also one of the most significant barriers to telehealth implementation because it leads medical organizations to mistakes with scaling and optimizing their software. Even though such flaws may initially seem insignificant, they may cause immense expenses when it appears necessary to modernize the existing software or scale it.
Hiring experienced technology professionals is the most cost-efficient solution for reducing the cost of telemedicine implementation. Experienced engineers can bring fresh insight into the project and help healthcare providers save money. Unfortunately, building a full-fledged in-house tech team and managing their workload is quite challenging and costly.
We see more and more healthcare providers picking an alternative to build in-house teams – outsourcing to experienced software development companies. This type of product development delegation allows companies to reduce the cost of telemedicine projects by 50% and more. In this approach, a tech partner organizes the recruitment process and assembles a tech team. Experienced software development companies can tune in on any stage of the software development lifecycle and provide the most cost-efficient technology solutions for clients. It concerns both choosing an optimal stack for the software development lifecycle and enforcing the client’s project with ideas and insights that allow for saving costs.
2. Scaling your software
Scaling is one of the most common needs of organizations that aim to embrace the potential of software development. The healthcare industry is not an exception. You may launch a top-notch medical information app oriented on a specific number of users, but, in some time, your user base may grow dramatically. The situation with the outbreak of COVID-19 is a vivid example of how there may appear an unprecedented growth in demand for medical services. In such a situation, your product can fail to cope with the growing data loads.
A healthcare provider that wants to avoid scaling barriers to telehealth while launching an application has to ensure the product’s scalability during the initial stages of its development. A relevant solution relies on software development specialists applying the most appropriate technology stack to deliver products that can be easily scaled up or down. While outsourcing the development of your telemedicine application to an experienced company, you receive highly scalable software. You may get a reliable partner handling all post-launch stages, such as application optimization and modernization.
3. Ensuring patient information security
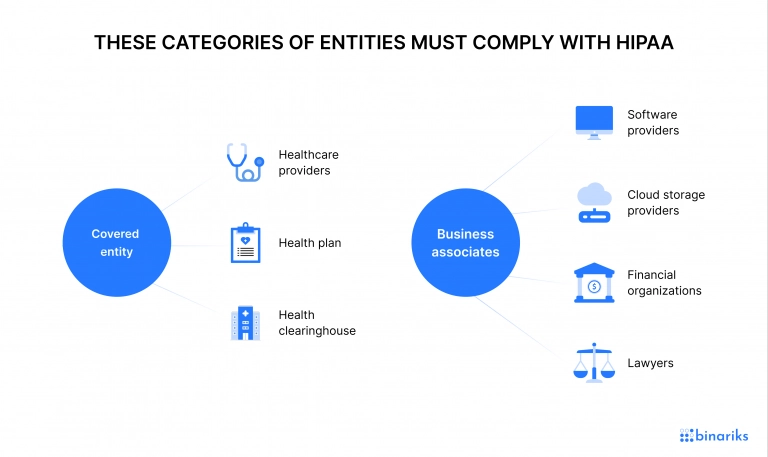
Information security is one of the most important points of telemedicine apps. All healthcare providers that operate with patients' private health information (PHI) must comply with HIPAA.
Ensuring secure telehealth proves to be a challenging task. Secure user verification protocols and complex data encryption are essential, but they are not enough to protect your application from potential data leaks. There are many more steps that have to be taken to ensure complete telemedicine HIPAA compliance.
Top-notch security of your medical information app requires you to establish multiple telemedicine security safeguards that may be challenging to implement. Another essential point is to avoid common mistakes, such as the lack of an adequate understanding of security or the reliance on outdated standards for storing healthcare information. You also must ensure that software development specialists working on your telemedicine application adhere to all confidentiality and data protection requirements.

Traditionally, developing telemedicine security safeguards comprises three consecutive steps:
- preliminary risk assessment
- elimination of the identified security threats
- security maintenance
Many medical companies handle those steps by outsourcing the product development to an ISO-certified technology partner. A reputable software development company will create a HIPAA-compliant product that can be used to secure PHI storage. Also, such a technology partner will grant you the confidentiality of all private information, which is also a significant benefit in terms of secure telehealth.
AWS-based Primary Care Platform
Binariks helped scale a web platform for patient monitoring and management
4. Design thinking in healthcare
One of the most significant facts about telemedicine apps is that they are often oriented toward both healthcare practitioners and patients. As long as people interact with telehealth applications for healthcare with different purposes, they require distinctive custom interfaces. A company that launches apps in the medical field has to consider the requirements of both user categories to create convenient use designs with appropriate functionalities.
An organization interested in telemedicine app development must consider peculiarities of user categories. For example, if particular telehealth mobile apps are created for senior citizens, patient-centricity requires the developer to consider that they may feel uncomfortable with digital technologies. Such an application's interface must be as simple in use as possible. You should also consider telemedicine app development cost , we wrote a detailed post about this.
When it comes to creating a top-quality UI/UX design for telehealth applications, experience is what matters. Professionals with a proven record of successfully designing apps know all the underlying principles and challenges associated with design thinking in health care and patient centricity. It is also valuable to arrange a comprehensive step-by-step process that consists of collecting user requirements, thorough analysis and planning, and implementing the design.
While hiring a UI/UX designer with experience in working on apps in the medical field or outsourcing this function to a reputable technology company, you get an additional guarantee that your design will meet the expectations of its users.
5. Ensuring customizability and functionality
Another essential aspect of a healthcare app is providing relevant functionality that will fulfill all users' requirements. It provides an appropriate connection between doctors and patients and integrates functions that will enhance the product’s relevance. For example, a healthcare practitioner may require telemedicine software platforms to have analytical functions. There has to be an option for customizing the analysis to their requirements. Top-quality telemedicine information software should also be flexible enough to adapt to unstable workflows and complex requests.
Finally, a patient-centric design of a telehealth app for doctors requires considering that different patients may have distinctive conditions and disorders. Top-quality healthcare interfaces allow patients to customize them according to their profile, concerns, and health conditions. Such matters should be considered during the preliminary design of telemedicine software. A tried and trusted choice is to request a consultation of a professional.
A technology partner will help a healthcare provider anticipate end-users needs and technically appropriate the product to their requirements. Another valuable point that can be implemented with the help of a technology expert is leaving a telehealth application open to further optimization and modernization. A dynamic product will adapt to new requirements, while its functionalities will be expanded once required.
6. Alternative to attending the hospital
Patients are unlikely to live close enough to your office to stroll there. This indicates that your patients travel 20, 30, and even 50 minutes to visit you. Some patients from rural areas wait until they are in dire need of care before scheduling an appointment because of their distance from your office.
You can communicate with patients via telemedicine solutions from any location using safe, live video conferencing and interact as if they are physically present by using a camera to ask questions, do basic examinations, and have conversations. Your patients can continue running errands right after the virtual appointment.
7. Accuracy of diagnostic
One of the primary issues with telemedicine is using digital instruments for patient examinations. Misdiagnoses can also occur in in-person healthcare, but employing remote care has a far larger risk.
CRICO's national CBS Database statistics show that 66% of telemedicine-related claims received between 2014 and 2018 are diagnosis-related. Additionally, according to 2019 Doctors Company data , the usage of telehealth technology is associated with an increase in medical malpractice lawsuits.
Inaccurate diagnoses might result in bad prescriptions, and potentially dangerous treatments also contribute to the rise in healthcare system expenditures. These problems prevent telehealth's widespread application among patients and doctors who desire to reduce the risk of medical mistakes.
Want to become HIPAA-compliant?
Learn about best practices of FHIR implementation.

How to ensure the privacy and security of telemedicine platforms
According to research , during a 10-year period in the U.S., there were 1,461 data breaches affecting the medical records of 170 million people.
Communication tools and techniques must be maintained securely to stop hackers or other threat actors from stealing PHI data. Telehealth privacy protection is crucial to ensure patient data confidentiality and safety.
So how can businesses improve the security of patient information with telehealth?
Provide secure solutions
Be sure to get security telehealth solutions that comply with HIPAA and access the most recent telemedicine cybersecurity features. You must also ensure your telehealth platform maximizes privacy and security compliance. This involves installing multi-factor authentication to reduce the likelihood that a security compromise may come from a stolen password alone.
Your staff should get training from the telemedicine cybersecurity consultants you engage with to ensure that everyone knows how to utilize your telehealth system safely. They should also conduct a thorough system evaluation to confirm that your telehealth system has been optimized for cybersecurity protection.
Use cutting-edge technology
Telehealth solutions must have a video conferencing function to connect with patients. Investing in technology will allow your practitioners to perform telehealth sessions without being interrupted by outdated or improperly integrated equipment.
If you want to enhance your telemedicine platform's capacity and provide a smooth user experience, look for opportunities to adapt apps to match the particular demands of your practice.
Create cybersecurity standards to safeguard PHI
Under HIPAA, it is mandatory to establish rules and arrange training in order to counteract security concerns in telemedicine andsecure PHI, regarding technology that manages PHI offshore.
Implement multi-factor authentication to increase PHI security and reduce the possibility of a security breach caused by a stolen password alone.
Assure endpoint security
Along with your workplace PCs, endpoints include phones, tablets, and laptops. These gadgets can pose security issues, particularly when utilized from home.
Secure these devices with telehealth security data encryption for all data transfers, especially when PHI is involved, in the interest of telehealth privacy and security.
Summary
Telemedicine software platforms are becoming necessary for healthcare companies that want to stay competitive. Unfortunately, the development of such software brings multiple telehealth issues, such as cost, scalability, security, relevant UI/UX design, and customizability. A tried and trusted solution for most challenges of telehealth is referring to experienced software development specialists. Outsourcing has become increasingly popular because it allows finding a dedicated team of developers with a proven record of web, desktop, and mobile telemedical projects at reasonable cost.
One of our successful cases of telehealth software is YourCoach. It is a full practice management platform and an operational environment. The client requested that YourCoach's digital solution be accessible through their web platform. The YourCoach team had to deliver an in-app experience to the client's end-users. Our engineers had to transform client’s application into an adaptive in-app experience into these applications.
Binariks is a company with an outstanding reputation in the market of telemedicine app development. We provide a broad range of services to SMBs and enterprises in the healthcare market. Make sure to check our portfolio for more specific information on our expertise. If you are looking for a cutting-edge medical application but are afraid of the significant challenges of telehealth, we provide you with a helping hand. Contact us to discuss your project and start gaining a competitive edge in the healthcare industry.
FAQ
Share

