Achieving seamless data exchange and Electronic Health Records (EHR) and Electronic Medical Records (EMR) interoperability is essential for any modern healthcare organization. EHR integration and EMR integration are paramount goals in the rapidly advancing landscape of healthcare technology, as they can dramatically improve how the whole organization system works.
At Binariks, we bring our first-hand experience in integrations to shed light on this critical aspect of modern healthcare. Through this article, you'll discover the core benefits of EHR integration, including enhanced data accessibility and streamlined workflows. We'll explore the role of healthcare application programming interfaces (APIs) in enabling seamless data exchange among various applications.
From common integration challenges to best practices for implementation, we'll equip you with the knowledge to navigate the integration journey successfully. So let's dive right in!
Core benefits of EHR integration
Integration with EHR systems offers many advantages backed by tangible evidence and real-world cases. Let's explore the core benefits healthcare organizations can derive from adopting integrated Electronic Health Records (EHR) solutions.
Streamlining healthcare workflow
Embracing EHR software integrations, medical and dental practitioners experience a streamlined clinical experience that expedites communication about care plans. By centralizing patient information on one platform, healthcare providers can collect, analyze, and share data more efficiently, resulting in a smoother patient journey.
In the review of empirical studies about the value of EMRs for hospital care published between 2010 and 2019, overall, 9/16 respective studies showed a reduction of costs (56%); 14/18 studies showed an increase of healthcare quality (78%) (Source ).
Enhancing patient engagement
Integrated EHR systems provide patients with relevant information and recommendations on their treatment stages. This fosters a more transparent doctor-patient connection, boosting patient engagement and commitm
ent to their healthcare institution. Access to health records from the comfort of their devices empowers patients to take charge of their health and reduces wait times for necessary information.
In the last decade, providing patients with online access to their medical records through a patient portal or mobile application has become an increasingly popular option which also helps to improve the quality of their engagement with their healthcare providers (Source ).
Ensuring protected health information (PHI) security
With HIPAA-compliant integrated EHR systems, patient data remains safe and protected from potential cyber-attacks. Transitioning from paper-based systems to EHR solutions ensures data integrity even in unforeseen incidents such as theft, fire, or natural disasters.
Improved healthcare outcomes
Physicians can deliver accurate diagnoses and informed judgments based on up-to-date patient information available on a single platform. An EHR-integrated system also facilitates a safer and more reliable means of issuing prescriptions, contributing to better patient care.
Anytime access to PHI
EHR integration enables seamless access to patient data from any device, ensuring more coordinated and efficient care. Everyone has access to up-to-date, correct patient information, whether the dentist is obtaining medical history information for treatment or administrators are accessing personal information to plan a follow-up therapy session.
Government Accountability Office (GAO) study shows that currently, approximately 90% of U.S. health care systems and providers offer patients online portal access to their EHR data (Source ).
Enhanced employee effectiveness
Integration with EHR automates organizational processes, freeing up valuable time for healthcare professionals and employees. This increased efficiency allows them to focus on providing excellent patient care and expanding their practice.
The adoption of EHR integration redefines the way healthcare institutions operate, leading to improved patient outcomes, higher patient engagement, and enhanced data security. These tangible benefits demonstrate the transformative impact of EHR integrations on modern healthcare practices, ensuring a more connected and patient-centric ecosystem.
Role of healthcare API in enabling clinical interoperability
Healthcare API (Application Programming Interface) is a set of standardized protocols and formats that facilitate the seamless exchange of healthcare data between different software applications and systems. It acts as a bridge, enabling healthcare providers to securely access and share patient information in real time, regardless of the underlying technology or platform used.
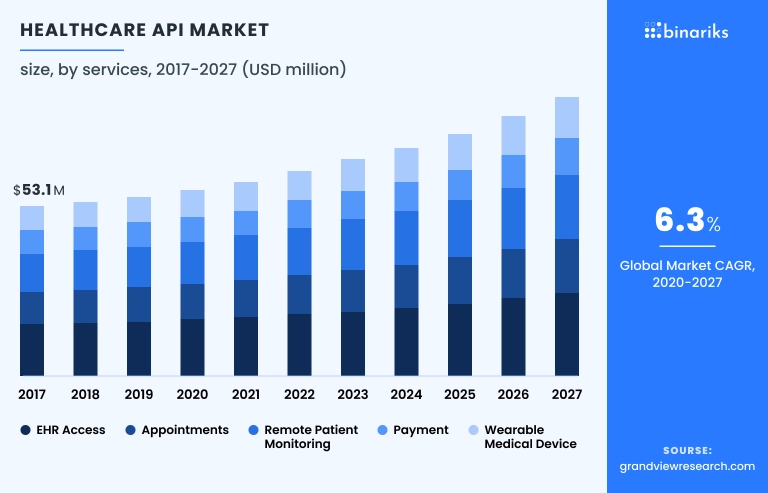
By adhering to industry-standard formats, such as Fast Healthcare Interoperability Resources (FHIR ), healthcare API ensures the accurate representation and interpretation of data, promoting data consistency and compatibility across various applications. And this is what clinical interoperability means.
Although actually software can be integrated through both APIs or file-based approaches, when it comes to healthcare solutions, APIs have emerged as a powerful tool and the number one choice. So, let's explore how exactly APIs enable clinical interoperability.
Streamlined data exchange
Healthcare APIs facilitate seamless data exchange between various systems, regardless of the vendor or platform. By integrating different applications through APIs, healthcare organizations can eliminate data silos and ensure that relevant patient information is accessible to authorized stakeholders when and where it is needed.
This streamlined data exchange leads to better care coordination, reduced duplicate efforts, and improved decision-making for patient treatments.
Enhanced care collaboration
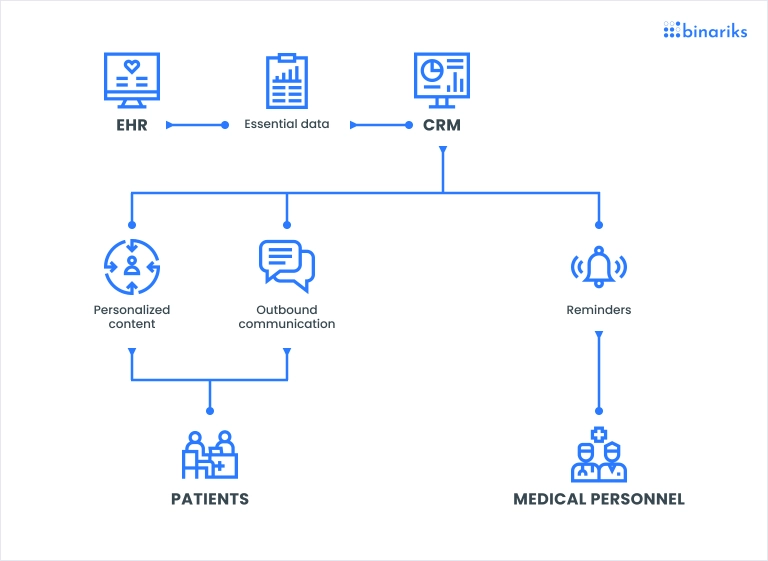
EHR API or any other healthcare software integration enables multidisciplinary care teams to collaborate more effectively. Physicians, specialists, nurses, and other healthcare professionals can access a unified view of patient data, allowing them to work cohesively on care plans and treatment strategies.
Enhanced care collaboration fosters a patient-centric approach, where the entire healthcare team is aligned in providing the best possible care for the patient.
Improved data accuracy and integrity
Integrating healthcare applications through APIs helps maintain data accuracy and integrity. When information is seamlessly exchanged, the likelihood of data entry errors or outdated records is reduced. This ensures that healthcare providers work with the most recent and reliable patient data, contributing to safer care delivery and better health outcomes.
Real-time access to critical information
Healthcare API integration allows healthcare providers to access critical patient information in real time. This is particularly vital in emergencies or when patients receive care from multiple providers. Immediate access to up-to-date patient data allows quicker diagnosis, timely interventions, and more informed medical decisions.
Increased efficiency and cost savings
Integrating healthcare systems using different EHR or EMR APIs streamlines administrative processes and reduces manual data entry tasks. This increases operational efficiency and cost savings by minimizing paperwork and manual errors.
Moreover, a more efficient workflow allows healthcare professionals to focus more on patient care, improving overall productivity.
Support for innovative healthcare solutions
Healthcare APIs open doors to innovation by enabling third-party developers to create new applications that can integrate seamlessly with existing EHR and EMR systems. This fosters a robust ecosystem of healthcare solutions, expanding the capabilities and functionalities of healthcare technology to serve patients and providers better alike.
The role of EMR/EHR integration in enabling clinical interoperability is pivotal in achieving a connected healthcare landscape. Through streamlined data exchange, improved care collaboration, and real-time access to critical information, APIs pave the way for enhanced patient care, increased efficiency, and the continuous growth of innovative healthcare solutions.
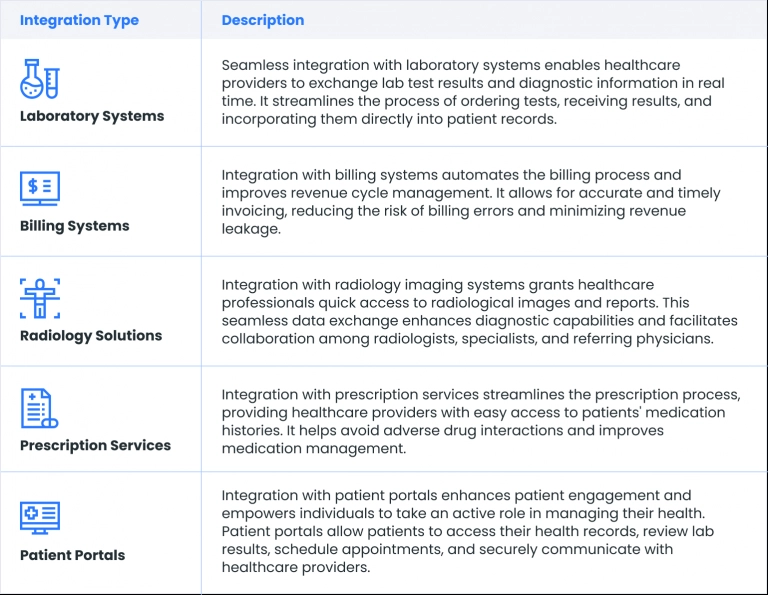
Essential EHR/EMR integrations
Integrating EHR APIs and other healthcare applications is vital for creating a comprehensive and interconnected healthcare ecosystem. Here are some essential EHR/EMR integrations that healthcare organizations should consider:
EHR/EMR integration challenges
EHR or EMR integration allows for building a comprehensive healthcare system and uniting multiple teams. A healthcare organization becomes more effective while the quality of care improves. Integrated right, your system can increase the EHR ROI and yield long-term benefits.
Sometimes the integration process is tricky. It implies many barriers you should consider:
- Inconsistent data: Combining data from multiple applications in one system, you will face formatting difficulties. It will be necessary to convert thousands of records from one format to another to merge the information. Besides, you will need to become FHIR compliant (the FHIR standard requires using XML or JSON data formats).
- Third-party technologies: To ensure EHR data interoperability, you will need to connect vital sign monitors, wearable devices, insurance systems, analytics platforms, and other solutions. Each of them has a different technological stack and integration requirements. Hence, the integration of third-party technologies poses certain complications.
- Software integration can complicate EHR user experience: Four out of ten physicians believe EHRs don't help their work and bring more challenges than benefits. If you additionally integrate them with third-party software, the navigation can become even more complicated. Hence, it’s important to complete integration carefully, regardless of whether you choose Epic, Cerner or Meditech , or any other system (Source ).
- Security and regulatory issues: Apart from purely practical advantages, proper EHR and EMR integration are required by law. HL7 FHIR and USCDI interoperability standards are changing the healthcare regulatory landscape for the next decades. If you are late with FHIR implementation , get ready for penalties.
The maintenance of such a complex system needs continuous tech support and updates. Note: it might be a problem if you don’t have qualified tech experts on your team, especially in the healthcare industry, where patient data and service are extremely valuable.
What regulations and standards apply to EHRs?
Learn about best practices of FHIR and HIPAA implementation.

Best practices for EHR integration
Integration of EHR into existing healthcare systems can be a complex undertaking, but with the right strategies and best practices, healthcare organizations can achieve a perfect result. Here are some recommendations to focus on during the EHR integration process.
1. Thorough planning and analysis
Before initiating the integration, conduct a comprehensive analysis of your current healthcare systems, data workflows, and specific integration requirements. Involve key stakeholders, including clinicians, IT teams, and administrators, to identify integration goals, potential challenges, and desired outcomes.
Thorough planning ensures that the integration aligns with your organization's objectives and minimizes disruption during the process.
2. Selecting the right EHR system
Choose an EHR system that is compatible with your existing healthcare applications and aligns with your organization's unique needs. Evaluate various EHR vendors, their features, interoperability capabilities, and data security measures.
Opt for an EHR solution that offers robust EMR system integration capabilities through standardized APIs, making the integration process smoother and more efficient.
3. Data standardization and quality assurance
Ensure that the data to be integrated is standardized, accurate, and complete. Inconsistent data formats and quality issues can lead to errors and hinder interoperability. Implement data cleansing and quality assurance processes to clean and validate data before integrating it into the EHR system.
This step is crucial for maintaining data integrity and reducing the likelihood of errors during the integration process.
4. User training and adoption support
A successful EHR integration involves not just technical implementation but also user adoption. Provide comprehensive training to healthcare professionals and staff members to familiarize them with the new system and its features.
Offer ongoing support and resources to address any questions or concerns, promoting smooth user adoption and minimizing potential disruptions to patient care.
5. Incremental rollout and testing
Consider adopting an incremental rollout approach, where the integration is deployed in phases. This approach allows for rigorous testing and evaluation of each integration phase, identifying and rectifying issues before proceeding further.
Conduct thorough testing to ensure that data is accurately and seamlessly exchanged between systems, and that all functionalities operate as intended.
6. Continuous monitoring and evaluation
Even after the integration is complete, continuous monitoring and evaluation are essential to ensure that the integrated systems operate efficiently and deliver the desired outcomes.
Regularly review system performance, user feedback, and data quality to identify areas for improvement and optimize the integration for better healthcare delivery.
7. Secure data exchange and compliance
Data security and compliance with healthcare regulations, such as HIPAA, are of paramount importance. Employ robust security measures and encryption protocols to safeguard sensitive patient information during data exchange.
Verify that all parties involved in the integration adhere to data privacy regulations, ensuring patient confidentiality is maintained throughout the process.
Here is an illustrative case:
Our client, a hospital, aimed to improve treatment outcomes and prevent aggravation in patients with CHD by harnessing deep insights from health data.
They envisioned a mobile app solution for continuous remote monitoring, measuring vital signs such as heart rate, saturation rate, respiratory rate, and blood pressure through smartphones using built-in sensors.
Ensuring secure data exchange between EHR/EMR systems and the application was a primary concern, requiring compliance with relevant state medical data security requirements, including HIPAA Rule.

Our solution involved developing a prototype app that utilized Photoplethysmography (PPG) to analyze vital signs using the smartphone camera and optionally an LED flash. Patients could measure key health indicators conveniently through their mobile phones, while ML CHF Processing technology enabled CHF status prediction and seamless communication with the hospital EMR system.
We divided the solution into app vendor and hospital sides, ensuring secure data access management for doctors and patients. As a result, we facilitated simplified vital sign monitoring for patients with chronic diseases, enabled HIPAA-compliant interoperability, and provided remote patient monitoring, especially beneficial for those with limited access to medical services during epidemics.
Cost to integrate EMR/EHR healthcare API
The EHR sector's growth is projected to reach $47.25 billion by 2027, indicating the increasing adoption and optimization of EHR integration in recent years (Valuates Report). Selecting, implementing, and optimizing EHR systems play a vital role in successfully managing clinical activities and patient load (Source ).
For multi-practice groups, licensing an EHR typically incurs costs ranging between $100,000 and $200,000, with additional expenses like high first-year maintenance fees. Migrating data from traditional platforms to an EHR may also result in supplementary expenses.
The most widely used EHR solutions include Epic, Cerner, and MEDITECH, accounting for the largest market shares in the US (Epic - 34.05%, Cerner - 23.71%, MEDITECH - 14.67%). These systems ensure high interoperability, facilitating easy FHIR implementation and compliance.
API implementation can have a significant impact on the cost of integrating EMR/EHR systems and can bring about various cost-saving benefits. Here are some ways in which API implementation affects the cost.
Reduced custom development
APIs provide standardized and pre-built interfaces, allowing healthcare organizations to connect and communicate with EMR/EHR systems seamlessly. As a result, the need for extensive custom EHR/EMR interface development is eliminated.
Developing custom interfaces from scratch can be time-consuming and expensive, requiring specialized expertise and ongoing maintenance. By leveraging APIs, organizations can bypass these costs and accelerate the integration process.
Lower maintenance costs
With APIs, the burden of maintaining custom interfaces is transferred to the API provider. API vendors typically take care of updates, and bug fixes, and ensure compatibility, saving healthcare organizations from incurring additional maintenance costs.
This shared responsibility for maintenance can free up resources and IT personnel to focus on other critical tasks.
Reduced EHR vendor interface fees
Some EHR vendors charge additional fees for integrating third-party applications or systems with their platforms. When using APIs, these integration fees may be reduced or even eliminated. APIs foster interoperability and allow for easier data exchange, making it more appealing for EHR vendors to encourage API integration.
Consequently, healthcare organizations can avoid costly vendor fees associated with custom integrations.
Conclusion: How Binariks can help
In conclusion, the seamless integration of EHR and EMR systems is crucial for achieving efficient healthcare operations, improved patient care, and enhanced clinical outcomes. As the EHR sector continues to grow, healthcare organizations are increasingly seeking reliable partners to navigate the complexities of EHR integration.
At Binariks, we have solid experience in EHR integration, with a deep understanding of the challenges and opportunities that come with this transformative process. Our team of skilled developers and healthcare IT specialists can assist healthcare providers in harnessing the power of EHR/EMR API integrations for streamlined data exchange, interoperability, and enhanced patient engagement.
With a proven track record of delivering innovative interoperability solutions in healthcare , Binariks is a trusted partner in navigating the intricacies of EHR integration. Let us help you unlock the full potential of your business and drive your journey towards a connected and patient-centric healthcare.
FAQ
Share

