Implementing a healthcare management system and having it unchanged for decades would be nice. Yet, healthcare solutions are too complex and demanding for that. After some time, they become outdated and cannot perform as well as they used to.
Only a professional EHR software development plan can enhance their productivity. If done right, the transition to a newer and more robust infrastructure allows healthcare organizations to use medical records with maximum efficiency.
Would you like to learn more about EHR data migration to a new system? Read about the data migration for EHR/EMR steps, best practices, and challenges below.
When an organization may need a successful migration of EHR data
EHR data migration has become a ubiquitous process in healthcare. Hence, almost every organization will have to migrate existing data to a new EHR at some point. So, when is the right moment to move your records?
Here are the main cases:
You'd like to change your current EHR vendor
If you have implemented electronic health records but don't like how the system works, you may decide to change it. In this case, EHR data migration is essential to transfer the records.
You switch an EHR to get the system with better functionality
Although you can integrate the missing features without changing the system, the limitations of legacy software may become a significant obstacle. That's when you will need to consider alternative vendors or analytics platforms for full transition and enhanced ROI for EHR software .
Your healthcare facility is going through acquisition
When two healthcare organizations merge, the acquiring one dictates the rules. Your entity may have to go through the EHR data migration process to unite with a large provider and form a single system.
You need to meet new regulatory requirements
If your existing EMR integration solutions are outdated, they may fail to comply with the latest healthcare and data processing regulations. In this case, the transition to another system is a way out.
Want to become HIPAA-compliant?
Learn about best practices of FHIR implementation.

What EHR system data can be migrated?
An EHR data migration tidies up data and examines access, utility, and backup policies. What patient data might be migrated typically?
- Allergies
- CT, MRI, and other radiographic images
- Contact information
- Insurance information
- Immunization history and dates
- Medical history
- Medical treatment plans
- Past and current medical diagnoses
- Past and current prescription medications
- Results of laboratory testing
Data migration options for electronic health systems
The healthcare data migration tools you choose will be strongly influenced by the amount of migrated data, its quality, your budget, and plan. Here are several options for migrating your EHR data:
- Transfering of CCD files, reducing the possibility of sending incorrect data
A CCD's objective is to increase communication between healthcare providers, such as when a patient goes to another provider. CCDs files contain care summary information.
- Starting from scratch with no CDD files
EHR allows you to export easily to a CCD clinical document from within the patient’s chart. As the clinical documents contain structured and unstructured patient data and can be used to support health information exchange with other EHR systems, at the beginning, you may decide whether to migrate CCD files or not.
- Removing obsolete, duplicate, and inactive dates
By adjusting and removing unnecessary data, healthcare organizations relieve the in-house work processes and communication with patients.
- Data simplification
Still, you can save time and money by getting hands-on with the software system and making patient and staff data as simple as can in your medical practice to ensure everyone is on the same page.
- Avoiding entering clinician data
In the healthcare industry, improving the overall quality and avoiding flowing clinical data is critical to guaranteeing excellent care and proper decision-making.
5 EHR data migration steps
Finding the right approach to EHR data migration takes a lot of research and experience. You must ensure custom healthcare interoperability of every component, prevent critical data loss, and consider many other nuances.
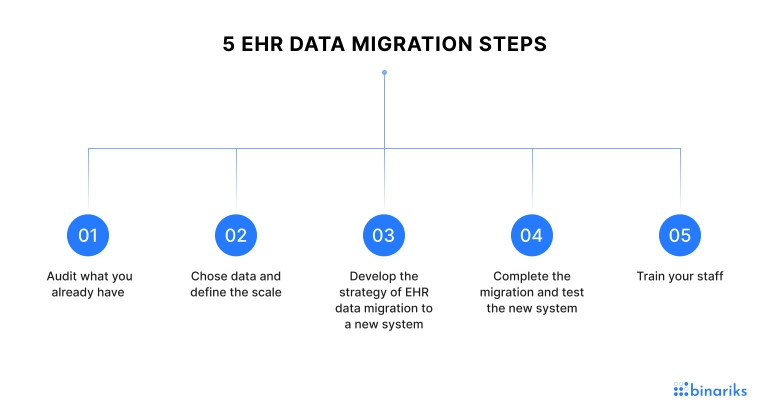
Below are the most critical steps of migrating an EHR data system.
#1. Audit what you already have
Before making any technical changes, you must know what data and human resources you currently have. In particular, it's essential to define whether your current IT staff can handle EHR data migration or you need to outsource this process. You must also estimate your budget and the expected time frame to plan the next steps.
For example, if you need to migrate records within the shortest time and don't have the necessary specialists on board, outsourcing will be the only option. It will allow you to avoid the recruitment stage, save money, and do everything faster.
#2. Chose data and define the scale
If you have been in a business for a while, chances are you might not need all the historical data. Your system may store outdated patient records you will no longer need for practical and legal reasons.
Hence, you must choose what information to incorporate in the EHR data migration process. Besides, you should also decide on future data uploading and processing practices.
Here are some questions you must find answers to:
- How much historical data do you need to convert?
- How much data do you need to hand-code, scan, and make structured in other ways?
- Will scanned documents be accessible as scanned images or searchable?
- Would you like to become completely paperless?
- What are your plans for the future, including the volume of provided services?
- What data can you leave behind without harming your practice and patients?
Planning to move your EHR data? Look how we can help!
#3. Develop the strategy of EHR data migration to a new system
Once you know what data to migrate and how to process it, plan the migration. Mind that it's a complex process that takes time, so you will need to move slowly. Start with the newest and most relevant records and move backward. Set timelines to control the process.
If you delegate EHR data migration to a third party, they will take responsibility for this stage and run the migration. You will only have to monitor the process.
#4. Complete the migration and test the new system
While EHR data mapping and migrating, ensure all the information is in the right place. Missing data is the main problem with moving to a new system, so be careful with it. Test the accuracy by double-checking patient names, dates, financial details, and other critical info. If there are any issues, immediately fix them.
#5. Train your staff
Global software changes may disrupt internal operations if the staff lacks the skills to use the new system. Hence, you must educate every team member on the updated data processing practices. You should also explain to them why EHR data migration was necessary since people usually resist changes.
Web and mobile apps for CareBridge
Binariks delivered electronic visit verification platform.
EMR data migration best practices
Successfully migrating EMR requires careful planning, execution, and follow-up. Below are the key best practices to ensure a smooth migration process.
Pre-migration best practices
- Gain a full understanding of your data: Assess your current system to map data structures, identify inaccuracies, and prioritize essential records for migration.
- Define scope and goals: Focus on necessary data for migration, avoiding unnecessary historical data. Clearly define business objectives and the migration’s scope.
- Choose the right migration platform: Select a platform that meets regulatory standards (e.g., HIPAA) and supports interoperability with systems like HL7 and FHIR.
- Prepare data for migration: Clean and organize data. Conduct a test migration to identify any issues before proceeding with the full migration.
During migration best practices
- Perform migration during off-hours: Minimize disruptions by scheduling the migration during non-peak times, ensuring smooth ongoing operations.
- Monitor the migration process: Continuously monitor the data migration to ensure that all records are transferred accurately. Keep an eye on data integrity and catch potential errors early.
- Communicate with stakeholders: Keep all stakeholders informed about the migration process, address any concerns, and provide updates to ensure alignment.
Post-migration best practices
- Validate data post-migration: After the migration is complete, thoroughly test the data to ensure accuracy, consistency, and completeness across all records.
- Update documentation: Revise all relevant documents, such as data dictionaries, user manuals, and workflow guides, to reflect changes made during migration.
- Train staff on the new system: Provide comprehensive training to ensure employees are familiar with the new system and understand updated workflows.
- Monitor data quality: Continuously check data quality post-migration to catch any inconsistencies and ensure long-term accuracy and reliability.
Following these practices will help healthcare organizations execute a successful EMR data migration while minimizing risks and ensuring a seamless transition to a more robust system.
Key strategies for EHR data migration
When you merge your healthcare company or acquire another one, there are high chances that you will need to plan a data migration between electronic health record (EHR) platforms. Given the present challenges in healthcare businesses, completing data transfers quickly and successfully is even more critical.
- Clean up patient record duplicates before migration
Before beginning healthcare data transfer, EHRs such demand a patient duplication rate of less than 3%.
According to the American Health Information Management Association , the typical patient record duplicate rate is between 8% and 12%, far from the 3% required. When hospitals attempt to communicate information across various EHRs (even ones from the same manufacturer), that number rises to 50% - 60%.
In a merger and acquisition situation, patients included in soon-to-be-legacy EHRs are likely to have visited or are active patients of the acquiring health system. Mapping old EHR patient IDs to correct information in the new EHR is time-consuming, error-prone, and costly. This sort of data mapping necessitates human validation and remediation of possible matches by your health information management (HIM) team. For a bigger healthcare business, this effort may take days or weeks.
Data migration suppliers collaborate to fix patient identification mapping and duplication concerns after seeing this scenario several times.
2. Set your data archiving strategy early
Quite frequently, companies forget to include the data archiving phase in the EHR transition plan. It usually happens when the client’s team learns how expensive it is to make historical data available for collections, compliance, and/or research. In an emergency, the business can migrate all previous data into the new EHR, which will almost certainly exceed licensing capacity and result in a hefty expense. Alternatively, the customer can keep the historical data in older systems and pay total maintenance fees.
Working with a data archiving vendor is a more proactive and cost-effective choice. Vendor fees are generally one-tenth the cost of maintaining older programs. A vendor's archiving solution may be significantly easier for HIM employees and the IT team to use and keep.
3. Use constant semantics
The way health systems install EHRs varies greatly, even down to the level of data field naming. Minor assumptions regarding field names might cause difficulties with data mapping, effectively halting an EHR data migration.
Before doing data mapping for a healthcare business, find out
- whether each field's label is current and well-defined: Organizations frequently construct a field only to utilize it for an entirely different purpose.
- whether two or more data fields with the same name in various EHRs have the same meaning: Field definitions can change significantly between EHRs, especially if the versions are years apart.
The IT staff may fix name issues before data mapping begins by addressing these disparities.
Common EHR data migration challenges
As mentioned, hiring professionals for EHR data migration is a great option to avoid many related challenges. Transitioning to a more advanced system may be troublesome due to profound software and infrastructure upgrades.
Here are only some of the issues you may face:
Limited technology infrastructure
If you have the server-based legacy infrastructure, scaling and moving to another system may be more challenging. 23% of healthcare leaders name technology infrastructure limitations a significant barrier to effective data utilization.
Barriers that hinder effective data utilization worldwide
The transition to cloud architecture is the best way to solve the infrastructure and network problem once and forever. Healthcare cloud solutions ensure more flexibility in data storage, analytics, and other computing capabilities.
Lower data safety
Ransomware, intrusion, data theft, and blackmail are a considerable threat to most providers. When moving to another system, legacy data protection processes may stop working, contributing to errors and an increased risk of data breaches.
Unmet patient expectations
Although many healthcare providers shift to more modern systems to optimize internal processes, the patients' opinion also matters. If new tools have worse quality and usability than previous systems, a healthcare provider may lose a large share of the patient base. The change of an EHR will significantly affect patient experience, so meeting their expectations is another critical goal.
Inflated financial expenses
Based on recent research , getting a new EHR system costs from $250 million to $1 billion. There are many hidden expenses like losses resulting from physicians diverted from other duties. That's why you must choose the type of migration and calculate your budget very carefully, ideally, with professional help.
Leverage Binariks' expertise for seamless EHR data migration
We offer comprehensive EHR data migration services tailored to the unique requirements of healthcare organizations. Our approach covers every stage of the process, from pre-migration planning and detailed data assessment to mapping and seamless integration.
We ensure compliance with regulatory standards like HIPAA and FHIR , safeguarding patient information throughout the process.
With our team's extensive expertise in managing complex legacy system migrations and hybrid cloud architectures, we ensure seamless transitions, maintaining data integrity and minimizing downtime. We also optimize system scalability, ensuring your healthcare infrastructure can support future growth.
Contact us , and let us future-proof your healthcare infrastructure with our reliable expertise in EHR data migration.
FAQ on EHR data migration
Share

