Healthcare providers are under pressure to act fast. Despite rapid digital adoption in other industries, many still operate on outdated platforms that slow down workflows, increase costs, and expose sensitive data to breaches.
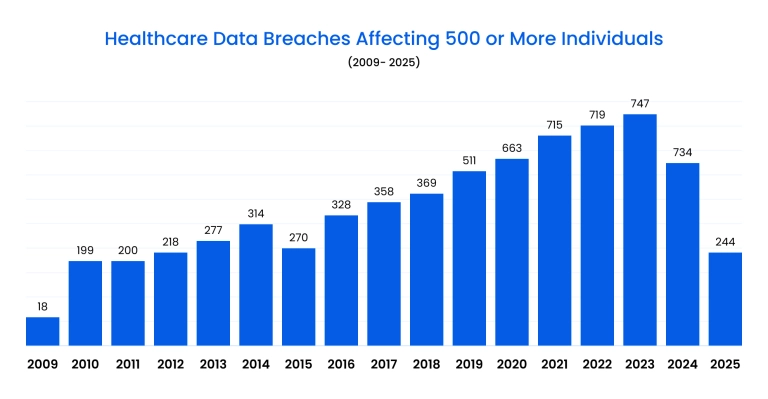
Reports show that in 2024 alone, more than 276 million patient records were compromised, highlighting just how dangerous lagging behind in healthcare software modernization can be.
According to Antino, modern IT systems cut medical errors by half and speed up patient processing by 40%. Yet 70% of providers still rely on outdated platforms, while 95% of executives call digital transformation a priority but admit legacy integration remains their biggest obstacle.
Outdated systems also struggle with compliance and create unnecessary bottlenecks for staff, leaving less time for patient care.
Updating a legacy healthcare system isn't just about replacing old tech but solving real business problems. Organizations that modernize see fewer medical errors, faster patient onboarding, and stronger regulatory compliance, while those that delay face mounting risks and higher long-term costs.
What you'll learn in this guide:
- What defines a legacy healthcare system, and why it matters
- How to recognize when your system is outdated
- The biggest challenges of running old software in healthcare
- Modernization strategies, technologies, and real-world case studies
Keep reading to understand how the right approach to modernization can protect your patients, optimize your operations, and future-proof your healthcare business.
What is a legacy healthcare system?
Legacy systems in healthcare are outdated applications or infrastructures that no longer meet modern performance, security, or compliance requirements.
They rely on old programming languages, unsupported databases, and rigid architectures that make integrating new tools difficult. This creates inefficiencies, higher maintenance costs, and compliance risks.
Common examples include:
- Electronic Health Records (EHRs) – old platforms with clunky interfaces, poor interoperability, and limited reporting functions that frustrate clinicians.
- Billing and claims systems – outdated financial software that slows reimbursement cycles and struggles with modern insurance standards.
- Scheduling tools – on-premise or legacy web apps that can’t scale or sync with other hospital systems, causing appointment bottlenecks.
- Laboratory and imaging software – rigid platforms that lack real-time data sharing and complicate diagnostic workflows.
- Pharmacy management systems – outdated solutions with weak integration and limited support for modern e-prescribing standards.
While these tools once served providers well, today they block effective healthcare modernization by making it harder to adapt to new regulations and patient expectations.
To overcome these challenges, providers often turn to custom healthcare software development to replace or transform outdated systems with scalable and secure solutions.
Types of legacy healthcare systems
Legacy platforms exist across multiple domains in healthcare, each creating unique operational and compliance risks. Below are the main categories providers most often need to address.
Electronic Health Records (EHRs) and EMRs
EHRs are the backbone of clinical operations, but many older systems are slow, complex to navigate, and lack interoperability. Poor design frustrates staff and disrupts patient care, while outdated infrastructure complicates upgrades and compliance.
Investing in the modernization of healthcare systems like EHRs delivers faster workflows, cleaner integrations, and improved patient outcomes. A real-world example is our legacy EMR modernization project that successfully rebuilt a behavioral health EHR without interrupting care.
Billing and claims processing
Financial platforms that haven't been updated often fail to meet current insurance and coding requirements. These systems generate delays, revenue leakage, and compliance headaches.
Understanding what a legacy system is in healthcare becomes clear when billing software can't adapt to new reimbursement models or automate claims effectively.
Scheduling and patient management systems
Many scheduling platforms still operate as stand-alone applications and cannot integrate with EHRs or telehealth solutions. This creates appointment backlogs, missed follow-ups, and poor patient experience.
Modernizing healthcare legacy systems allows providers to streamline access, improve coordination, and reduce no-show rates.
Laboratory and imaging systems
Diagnostic tools generate critical patient data, yet outdated lab and imaging software often restrict real-time sharing and analytics. These limitations reduce the speed of diagnoses and collaboration between specialists.
Replacing them with modern healthcare software enables secure integrations, better reporting, and scalable storage for medical imaging.
Pharmacy management systems
Older pharmacy software often lacks proper e-prescribing capabilities and integration with broader EHR platforms. This leads to medication errors, inefficient stock management, and compliance issues. Modern pharmacy systems enable real-time prescription monitoring, automated drug interaction checks, and safer patient care.
Telehealth and remote monitoring platforms
During the pandemic, many clinics adopted quick-fix telehealth tools that haven't kept pace with compliance or scalability needs. Legacy telehealth systems may lack strong encryption, interoperability, or the ability to handle growing patient volumes.
Updating these platforms ensures secure remote consultations, stronger patient engagement, and smoother integration with core clinical systems.
How to know if your healthcare system is outdated
Relying on legacy healthcare software creates hidden costs and risks that pile up over time. The challenge is that many organizations don’t notice the warning signs until inefficiencies and compliance problems start affecting patient care.
A practical way to check the health of your IT environment is to look at technical performance, user experience, and business outcomes.
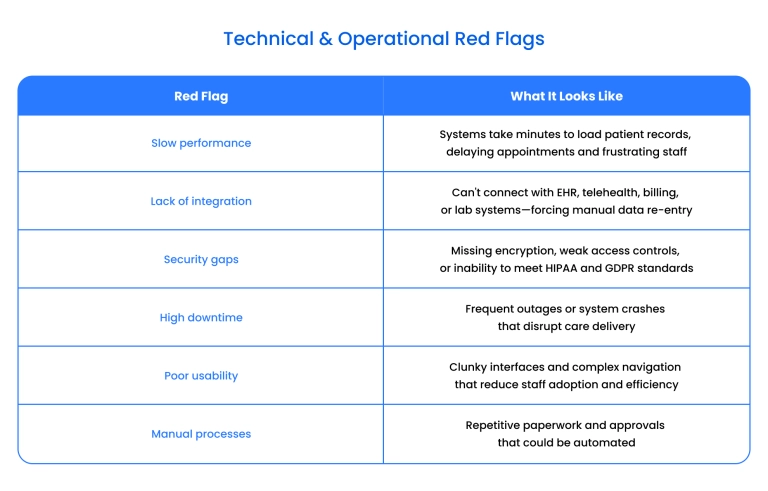
Business signals from legacy healthcare systems:
- Escalating maintenance costs – IT spending goes up while productivity gains stay flat.
- Compliance struggles – failing security audits or constantly scrambling to meet new regulatory requirements.
- Patient dissatisfaction – lower satisfaction scores linked to digital touchpoints such as portals, scheduling, or telehealth.
- Inflexibility – difficulty scaling to new locations, adding users, or adapting to new reimbursement models.
- Data blind spots – limited analytics and reporting capabilities that block data-driven decisions.
If multiple items from this checklist apply, it strongly indicates that your current systems are hindering progress. Modernization is not merely a technical upgrade; it serves as the foundation for scaling services, safeguarding sensitive data, and enhancing patient experience.
Key challenges of legacy healthcare systems
Healthcare organizations that rely on outdated IT face a dangerous mix of cost, inefficiency, and risk. Legacy healthcare systems create bottlenecks that slow down care delivery, frustrate staff, and weaken patient trust. What was once the backbone of operations has become a barrier to progress. The main challenges include:
- Escalating operational costs: Maintenance of obsolete platforms drains IT budgets through rising licensing fees, expensive hardware upkeep, and the need for specialized staff. These costs grow every year, while the value delivered by the system continues to decline.
- Integration barriers: Legacy platforms often can't connect with modern EHRs, telehealth tools, or lab systems. This creates silos of information, delays diagnoses, and forces staff to re-enter data manually, increasing the risk of medical errors.
- Compliance failures: Outdated systems struggle to meet regulatory requirements such as HIPAA or GDPR. They lack modern audit trails and data governance tools, making compliance reporting difficult and exposing organizations to penalties.
- Security vulnerabilities: Many legacy platforms were built before today's cyber threats existed. Without strong encryption, multifactor authentication, or continuous monitoring, they expose sensitive patient records to breaches.
- Workflow inefficiencies: Clunky interfaces and outdated user experiences waste valuable staff time. Clinicians spend more time navigating the system than treating patients, reducing productivity and increasing burnout across the workforce.
- Vendor lock-in: Older systems often run on proprietary technologies that vendors no longer support. This makes upgrades expensive and risky, leaving healthcare providers dependent on fragile and inflexible setups.
As mentioned in this study on enterprise architecture in healthcare , "these outdated systems, while once foundational to healthcare operations, now hinder the sector's ability to keep pace with technological advancements and the growing demands for interoperability, data-driven insights, and regulatory compliance".
Together, these challenges turn legacy systems from assets into liabilities. They undermine care quality and limit an organization's ability to innovate and grow.
Challenges in healthcare legacy system modernization
Replacing outdated IT isn't simple. While the goal is to move toward modernized healthcare systems, the process itself comes with risks that can disrupt operations, inflate budgets, or compromise patient data if handled poorly. Modernization must balance innovation with stability in a sector where downtime can cost lives.
The main challenges include:
- The risk of "rip-and-replace" modernization: Completely replacing old systems in one go often leads to cost overruns, staff resistance, and dangerous downtime. Healthcare organizations need phased approaches that minimize disruption and ensure continuity of care.
- Data migration complexity: Moving sensitive medical data from legacy platforms to modern healthcare systems is fraught with risks. Data corruption, loss of records, or incompatibility with new formats can create compliance problems and affect patient safety.
- Interoperability gaps: Even after modernization, new platforms must integrate seamlessly with labs, pharmacies, insurers, and national health registries. Achieving this requires strong governance and frameworks for data exchange.
- Security during transition: Shifting from on-premise to cloud or hybrid models introduces vulnerabilities. Without careful planning, sensitive health data may be exposed during migration, making secure practices like healthcare cloud migration essential.
- Change management and staff adoption: Clinicians and administrators often resist new workflows, especially if training is inadequate. Even modern platforms can fail to gain acceptance without strong onboarding and user-centered design.
- Cost management: Modernization projects frequently run over budget due to hidden technical debt, underestimated migration needs, or vendor complexity. Financial planning is critical to prevent spiraling expenses.
Each of these challenges must be anticipated early in the project lifecycle. The stakes are too high in healthcare to gamble with rushed or poorly managed modernization.
How to overcome modernization challenges
The risks of updating legacy healthcare IT systems are real, but they can be managed effectively with the right strategy. Successful projects don't rely on a single "big bang" replacement. Instead, they follow phased, well-governed approaches that reduce disruption and deliver value step by step.
Best practices for overcoming modernization challenges include:
- Adopt a phased modernization strategy. Instead of replacing everything at once, break the project into manageable phases. This ensures continuity of care while gradually introducing new features and retiring outdated ones.
- Prioritize non-disruptive transitions. Follow best practices for non-disruptive modernization, such as running new systems in parallel until staff are fully trained and data migration is validated. This minimizes downtime and builds user confidence.
- Focus on interoperability from the start. Design healthcare modernization solutions with open standards and APIs. This prevents new data silos and ensures that modernized systems can integrate seamlessly with external partners, labs, and insurers.
- Strengthen data governance and security. Modernization is the ideal moment to build strong frameworks for data quality, access control, and regulatory compliance. Address security proactively to avoid exposing sensitive patient records.
- Invest in user-centered design and training. Modernizing healthcare systems only works if clinicians adopt them. Intuitive interfaces, role-based workflows, and tailored training programs drive adoption and reduce resistance.
- Establish continuous monitoring and feedback loops. Use agile delivery models and monitoring tools to collect real-time feedback, track performance, and resolve issues before they impact operations.
By combining phased execution with strong governance and user engagement, healthcare providers can modernize effectively while avoiding the pitfalls that sink many large-scale IT projects.
Technologies and solutions for healthcare system modernization
Modernization involves more than just replacing old systems; it emphasizes creating a future-ready foundation.
Below are the core technologies driving healthcare transformation and ensuring long-term scalability.
Cloud infrastructure
Migrating to the cloud provides scalability, resilience, and reduced infrastructure costs. It enables providers to roll out new features quickly, ensure high availability, and improve disaster recovery. Secure deployments through private, public, or hybrid models also support compliance with healthcare regulations.
APIs and interoperability standards
Application Programming Interfaces (APIs) and standards like HL7 and FHIR are critical for seamless data exchange. They allow new and old systems to communicate, eliminate silos, and support integrations with telehealth, lab systems, and third-party health apps.
Artificial intelligence and machine learning
AI and ML unlock predictive analytics , clinical decision support, and personalized treatment recommendations. They help detect anomalies, flag high-risk patients, and automate routine tasks, freeing clinicians to focus on care delivery.
Microservices and modular architectures
Breaking large monolithic systems into microservices makes applications more flexible and easier to scale. This modularity allows teams to update or replace specific components without disrupting the entire system.
Advanced security solutions
Modernized healthcare platforms must embed security by design. Encryption, zero-trust frameworks, and role-based access controls protect sensitive patient data and ensure compliance with HIPAA, GDPR, and other regulations.
Data analytics and business intelligence
Advanced analytics platforms help providers extract insights from clinical and operational data. From identifying bottlenecks in workflows to predicting patient trends, BI tools turn raw data into actionable intelligence.
Telehealth and remote care platforms
Telemedicine platforms, patient portals, and remote monitoring tools extend care beyond the hospital. They improve access, reduce readmissions, and increase patient engagement – all while integrating smoothly with EHRs.
Future-proofing healthcare applications means designing with these technologies at the core. When combined strategically, they provide a scalable and secure ecosystem that supports innovation while maintaining compliance.
Benefits of healthcare legacy software modernization
Modernizing outdated healthcare platforms unlocks both clinical and financial value. Organizations that replace or transform legacy systems see faster operations, improved compliance, and stronger patient outcomes.
Key benefits include:
- Operational efficiency – streamlined workflows and reduced manual tasks save staff time.
- Regulatory compliance – modern platforms embed security and governance to meet HIPAA, GDPR, and local standards.
- Cost reduction – lower maintenance expenses and fewer system outages cut long-term IT spending.
- Better patient experience – improved usability, faster service, and digital engagement boost satisfaction.
- Scalability and innovation – flexible architectures make expanding services and adopting new technologies easier.
Real-world examples of legacy healthcare system modernization
Modernization isn't just a theory – healthcare organizations worldwide are already tackling outdated platforms with varied approaches. These cases highlight the practical challenges and measurable results of moving beyond legacy technology.
- Meuhedet: Legacy → Cloud & remote monitoring
Israel's Meuhedet health organization retired local databases and migrated core IT workloads to the cloud. They also launched a remote patient-monitoring center integrated with their legacy EMR to support COVID-19 patients, proving even entrenched systems can evolve.
- Springer: Hospital HIS migration
A study on a hospital's shift from a 20-year-old HIS to a web-based platform revealed the scale of migration challenges. Issues included data integrity risks, staff resistance, and inter-department integration struggles.
- Nature: Robotic process automation in healthcare
A case from Taiwan applied RPA to automate medical claims within a legacy healthcare setup. Modernization has cut administrative burdens, reduced errors, and accelerated claim approvals without replacing the entire system.
These examples show that modernization can take many forms, from cloud migration to system replacement or targeted automation. What unites them is the outcome: lower costs, better workflows, and improved patient experience.
Our case study: Modernizing EHR without disrupting care
While industry reports highlight the risks of legacy systems, the most convincing evidence comes from real-world projects.
Our recent project for the patient management system for clinicians shows how a behavioral healthcare provider successfully modernized its EHR without disrupting patient care.
Challenge
Our client, a behavioral healthcare software provider, relied on legacy EHR systems that had become inefficient and difficult to maintain.
Their platform suffered from poor usability, complex navigation, and outdated interfaces that frustrated staff and practitioners.
The obsolete tech stack created compliance risks, integration hurdles, and limited scalability. Inefficient manual workflows consumed valuable time, while the system struggled to keep pace with evolving regulatory standards.
Solution
Binariks designed a full EHR modernization strategy to rebuild the platform from the ground up.
The process started with structured requirements elicitation, followed by scalable technical architecture design, sprint-based agile development, and comprehensive QA. We assembled a cross-functional team of healthcare specialists, cloud engineers, and UX designers to ensure compliance and user-centered design.
The implementation rebuilt the platform from the ground up with modern technologies:
- Backend: .NET 8 for secure and high-performance operations
- Frontend: React for responsive, intuitive UI
- Cloud: Azure for scalability and compliance readiness
- Database: PostgreSQL for reliable data management
- Security: Auth0-based role access, Azure Key Vault, multi-tenant data isolation
- DevOps: Kubernetes, Terraform, CI/CD pipelines, Azure Application Insights, Grafana dashboards
- Testing: Playwright-based automation combined with manual clinical workflow testing
The architecture was designed as modular and service-oriented, enabling independent scaling and minimizing disruption during deployment.
Check out full project details in our Theramanager case study .
Results
The modernized platform addressed all major pain points. Daily operations became smoother thanks to redesigned workflows and improved UX, increasing adoption across practices.
New integrations with behavioral health services, such as Open and Dr.First, eliminated data silos and supported better patient coordination. Compliance was reinforced with advanced security measures and granular role-based access controls.
Additional benefits included automated tenant onboarding that shortened setup time, advanced monitoring and alerting that improved reliability, and DevOps-driven automation that reduced maintenance overhead.
The result was a future-proof system that solved immediate issues and provided a strong foundation for ongoing growth and service expansion.
Conclusion
The risks of running on legacy platforms in healthcare are far from theoretical – they directly affect patient care, compliance, and financial stability. Modernizing these systems ensures providers stay competitive, secure, and prepared for evolving regulatory standards.
Binariks has proven experience guiding healthcare organizations through complex modernization projects without disrupting daily operations. If you're ready to upgrade your infrastructure, our team can help design and implement solutions tailored to your workflows and compliance needs.
Explore our healthcare expertise to start your modernization journey.
FAQ
Share

