The implementation of FHIR brought a lot of confusion in the healthcare industry, and FHIR vs. HL7 caused questions among users.
The companies that used HL7 V2 and other versions started to question what requirements to follow now. Here is a short answer: Although all these standards implement interoperability, HL7 FHIR is considered the most innovative. Unlike the older standards, it employs open web technologies and RESTful web services that simplify the integration of multiple system components.
Still, both HL7 V2 and FHIR implementation is challenging and requires specific expertise. Since Binariks has already assisted many healthcare providers with FHIR adoption , you can use our services to outsource this task.
Here is the short comparison of HL7 V2, HL7 CDA, and HL7 FHIR:
| Factor | HL7 V2 | HL7 CDA | HL7 FHIR |
| Nature and Design | Messaging standard using pipe-delimited text. Event-driven. | XML-based standard for clinical document exchanges. | Modern, web-based standard with RESTful APIs. XML or JSON "resources" for exchange. |
| Interoperability | Limited. Requires custom interfaces for each implementation. | Standardized document structure, but may need system mapping. | High. Simplified data exchange with predefined resources. |
| Adoption and Usage | Widely adopted globally. Used in older systems. | Used for specific cases like EHR summaries. | Rapidly growing adoption due to modern architecture. |
| Flexibility and Extensibility | Highly flexible but can lead to inconsistent implementations. | Standard way to represent clinical documents. | Modular and extensible by design. Can combine resources for complex scenarios. |
This article should help you understand the difference between HL7 and FHIR. Read the comparison to figure out which option you need.
The key difference between HL7 and FHIR
The main difference between FHIR and HL7 is that FHIR leverages RESTful web services and open web technologies such as XML, JSON, and RDF, while HL7 only supports XML. FHIR builds on previous standards, including HL7 CDA, V2, and V3, but is easier to use since it covers a broader range of technologies.
Besides, FHIR is rich in options for exchanging data among systems. It supports the RESTful API approach that replaces point-to-point interfaces with one-to-many interfaces. As a result, data exchange happens more smoothly and the time needed to onboard new data exchange partners reduces. In this respect, the previous HL7 standards are more outdated and less versatile.
Why is the HL7 FHIR concept used?
When referring to FHIR, you will likely encounter the term HL7 FHIR, essentially the same thing as FHIR. This is a perfectly viable term because the FHIR standard was developed by HL7 (Health Level Seven International). Therefore, FHIR is always an HL7 standard, but not all HL7 standards are FHIR.
FHIR is considered the latest and most modern standard by HL7. However, it's worth noting that HL7 has other standards, like HL7 V2.x and HL7 V3, which are different from FHIR and serve similar but distinct purposes in healthcare interoperability. We will discuss all of these standards in more detail in this article.
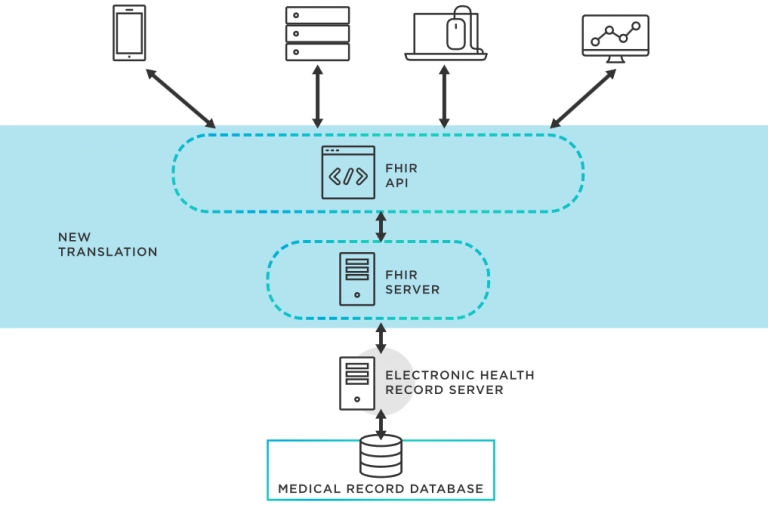
FHIR HL7 standard uses API so different applications can tune in to the main operating system and receive information from there. Here is how it works:
A brief overview of HL7 and FHIR
HL7 and FHIR standards appeared in the healthcare industry because of the need to connect the growing number of software solutions. The first HL7 protocol appeared over thirty years ago and evolved into what we now know as FHIR.
How the healthcare industry ended up with FHIR and HL7
The HL7 FHIR first appeared in the 1960s with the deployment of the first-ever health IT system. There were no interoperability standards back then. Yet, this event started the long history of healthcare systems.
(Source )
In 1987, Health Level Seven International (HL7) was founded to create standards for global healthcare data interoperability. In 1989, it released the HL7 V2 to ensure enterprise-level interoperability across the industry.
Since by the early 2000s, the role of data in facilitating clinical and medical workflows increased, the HL7 V2 data model could no longer offer proper methodologies and resources. It nudged the organization to develop a more complex messaging standard of HL7 V3 based on XML coding V3. It was not backward compatible with HL7 V2, so it didn't gain much popularity.
Two years after the HL7 V3 release, Health Level Seven International launched the Clinical Document Architecture (CDA) standard that was viewed as a simpler version of HL7 V3. It was an XML-based markup standard developed to enable an easy exchange of clinical documents.
After considering the limitations of the previous standards, HL7 released FHIR in 2014 as the simplest and most universal version of healthcare interoperability standards.
What Does HL7 Mean for Healthcare
When people speak of HL7, they usually mean V2 since this version has become widely used. So why do healthcare organizations need it?
Before HL V2, every interface connecting system had to be custom-designed. It means sending and receiving application vendors invested much time and effort in programming. As there were no standards for processing patient data, interface implementation was expensive. Most importantly, data exchange between healthcare apps was not always possible.
HL7 V2 changed that. This standard allows healthcare providers to connect versatile applications, systems, and devices more easily. It improves healthcare quality through integrated data and more advanced health analytics.
What Does FHIR Mean for Healthcare
The FHIR standard in healthcare can do everything HL7 V2 does and more. It eliminates the limitations of HL7 and has a less steep learning curve. FHIR is not limited to a single encoding syntax, unlike V2. It also has one-to-many data exchange capabilities, offers robust security functions, and cuts implementation time. Simply put, it makes adopting healthcare interoperability simpler. Vendors need less time to connect third-party apps and make them work as a whole.
If you want to supercharge the benefits of FHIR even more, consider using SMART on FHIR . SMART is an open-source API that allows engineers to build apps that can run anywhere in a health system.
Real using HL7 FHIR with examples
Here are several examples of how the FHIR HL7 standard works in real life. The first example deals with electronic health record (EHR) integration. Let's say hospital A uses EHR System X, and hospital B uses EHR System Y. These systems might have been designed without considering the need to integrate.
The FHIR HL7 standard can help in this situation. For an integration, Hospital A's EHR System X exposes a FHIR-compatible API. Hospital B can then use this API to pull specific FHIR resources for shared patients.
In another example, a diabetes patient uses a mobile health app to track their blood sugar levels and insulin doses. The app can interact with the patient's healthcare provider's EHR to pull and push information. The mobile app authenticates with the EHR's FHIR-compatible API. It retrieves resources from the EHR and then writes resources when the patient logs new data.
Core HL7 and FHIR protocols
FHIR and HL7 standards transmit information between system components based on the rules set by specific protocols. The main HL7 protocols you will work with include:
OSI Layer 7 Protocol
The Layer 7 protocol provides application services for network software based on HTTP, SMTP, and other level 7 protocols. It keeps the exact format and content that data healthcare apps exchange and has no connection with the mode of transmission between the apps. Usually, a TCP/IP connection is used to deliver messages.
Event Driven Protocol
Any healthcare-rated event that creates the need to exchange information between applications defines an event-level protocol. It may be a patient's admission to a facility or when a doctor forwards a medicine order to the pharmacy. So every time an app captures an event, it exchanges data with other systems that need it.
Application to Application Protocol
The protocol ensures the communication and data exchange between two independent apps, not between client-server type applications. In this case, the message they share is of utmost importance. The role of each app doesn't matter.
Standard Protocol
Two apps won't be able to exchange a message until a proprietary, non-standard link is created. HL7 standard protocol facilitates link building and prevents you from data exchange issues when you connect to a third-party system.
Exchange Protocol
This protocol determines how apps will transfer data to each other. Storage and data processing have no importance. Although the database structure needs to match HL7 message definitions, this is not mandatory.
Want to become HIPAA-compliant?
Learn about best practices of FHIR implementation.

Similarities between HL7 and FHIR
When choosing between FHIR integration or HL7, remember that it isn't a win-or-lose case. Actually, FHIR or HL7 have many things in common and can help you with the same interoperability tasks. Both belong to the family of HL7 standards and are launched by Health Level Seven International.
FHIR relies on the best features of HL7 V2, HL7 V3, and CDA but also takes into account the latest web technologies. Since HL7 V2 appeared several decades ago, it was developed without due attention to Internet technologies. They just weren't in use that much back then. FHIR fixes these flaws by offering a more modern version of HL7 standards adapted to the new reality of the highly digitized world.
It's worth noting that as V2, V3, and CDA versions of HL7 differ, they will also have different similarities with FHIR. Here we focus on HL7 V2 as the most widespread option.
When you compare HL7 V2 to FHIR, you will find out the following similarities:
Built around reusable "chunks" of code
The main idea behind HL7 standards is to provide software engineers with resources to achieve interoperability in healthcare systems. Developers have ready chunks of data they can use to build new systems faster.
Forward/backward compatibility
Both standards compared are backward and forward compatible. What does it mean? Backward compatibility is when readers with a newer schema can parse data from an older schema without errors and distortions. Forward compatibility means readers with an older schema can parse data from a newer schema. From a practical standpoint, forward/backward compatibility implies you can successfully use interfaces and data from other versions. It reduces the investment in hardware, software, and engineering.
Extensibility mechanism
With both FHIR and HL7 standards, you can extend existing systems by adding new functionality or modifying current features. The extensibility mechanism is essential in healthcare systems that require frequent changes. You can enhance what you have without impairing its work.
Comparison of FHIR with HL7 (V2, V3, and CDA)
Now that we have covered the similarities between FHIR and HL7, it's time to discuss the differences. Even though the key difference is that FHIR supports RESTful APIs and open web technologies while HL7 standards don't, there are many other things to consider.
This table should help you with the most critical difference between HL7 V2, V3, CDA, and FHIR.
HL7 V2 | HL7 V3 | HL7 CDA | HL7 FHIR | |
General Structure | Message | Structured message | Document | API |
Use cases | Medical record exchange | Medical record exchange | Clinical document exchange | Universal health data exchange, including apps, smart devices, and wearables. FHIR enables sharing medical records, individual patient data, provider data, and other data sources as needed. |
Platform | EMR, EHR, HIS | EMR, EHR, HIS | EMR, EHR, HIS | EMR, EHR, HIS, mobile apps, and wearables |
Flexibility | Flexible | Less flexible | Less flexible | Very flexible |
Message Format | Based on pipe and hat characters | XML | XML | XML/JSON, API-based access |
Interoperability Method | Syntactic | Syntactic and semantic | Syntactic and semantic | Syntactic and semantic |
Security | Transport layer security | Transport layer security | Transport layer security | Transport layer security and SSL |
Tools used | Parser | Model compiler | Model compiler | Only console and browser |
Compatibility | All V2 features are compatible | Not compatible with V2 | Not compatible with earlier versions | Backward compatibility with V3/CDA. Not compatible with V2 |
ICD use | Limited ICD support | Allows embedding ICD as an object | Allows embedding ICD as an object | Allows embedding ICD as an object |
LOINC use | Limited LOINC support | Allows embedding LOINC in RIM object | Allows embedding LOINC in RIM object | Allows embedding LOINC in RIM object |
DICOM use | Limited DICOM support | Allows embedding DICOM in RIM object | Allows embedding DICOM in RIM object | Allows embedding DICOM in RIM object |
Reliability | Less reliable due to many optional columns | More reliable due to many required data | More reliable due to many required data | More reliable due to the availability of specific resources that can handle particular data |
Implementation cost | Cheap | More expensive | More expensive | Cheap |
Popularity | Popular | Less popular | Popular | Still emerging but likely to become the leading standard |
Learning curve | Weeks | Months | Months | Weeks |
Summing up the FHIR and HL7 difference details, choosing the standard to implement interoperability depends on your existing resources and plans. If you want to stay flexible and open to innovations, FHIR is preferable. If you prefer well-established standards, other HL7 options may be more suitable. Binariks, as a healthcare development company, usually recommends FHIR. Find out what makes it so good below.
Why is FHIR better than HL7
Speaking of FHIR implementation advantages, it's worth starting with the fact that this is the latest HL7 standard. In other words, it uses everything that has been developed and tested before to offer the best interoperability capabilities. Health Level Seven International considered the flaws of the previous versions and adapted the new one to the demands of the current healthcare market.
FHIR outperforms other HL7 versions since it is:
- More convenient to implement than other standards. FHIR covers a wider variety of technologies and is easier to master. It has much better compatibility than V2 and focuses on helping software engineers to achieve interoperability without obstacles.
- Suitable for most common scenarios. FHIR resources provide software engineers with components they can use to build custom software. It's a foundation that allows developers to adapt the healthcare system to users' administrative and business needs.
- Freely available. You get free access to all resources necessary for FHIR implementation. It significantly cuts implementation costs.
- Supports multiple paradigms and architectures. Engineers have lots of flexibility in terms of tech solutions and the decisions they make. It allows you to achieve interoperability in highly complex and multi-component systems.
- Provides advanced data governance. With FHIR, healthcare providers and patients have more control over shared data. It allows you to increase data security while making information exchange easier.
These benefits give a convincing reason to choose FHIR rather than other standards. It makes healthcare organizations better adapted to rapidly changing interoperability requirements. Of course, FHIR is not perfect, but so far, it's the top option for many healthcare software developers.
FHIR implementation challenges
When we say you need prior experience to implement FHIR-based interoperability, we mean it. Healthcare systems include multiple components that may be challenging to connect. You will also have to study many HL7 FHIR specifications to ensure you meet the requirements.
Here is a brief overview of the main FHIR implementation challenges:
- For large organizations, the scope of FHIR coverage is extensive. Therefore, the implementation takes time and financial resources.
- You will likely face a lack of engineers who have experience with FHIR. Since this is a relatively new standard, the number of people who know how to work with it is limited.
- FHIR integration must be tailored to specific business needs. Each healthcare provider operates in a unique way and leverages different apps. That's why each implementation requires a custom approach.
- Security issues are sure to happen due to many data sources connected. Clinical data normalization and consistency across third-party apps are still tricky.
- Compliance is a never-ending story since you will need to integrate new apps as your software needs change.
- There is still a lack of visible case studies. As healthcare providers have only started the transition to FHIR, you will not have that many instructions on how it works.
For more detailed information on FHIR challenges , read the previous article from our blog. It explains why FHIR adoption may be problematic and how to overcome the most common issues.
If you want to avoid problems, you can take a shortcut to FHIR implementation and hire a professional healthcare development company. Healthcare interoperability providers like Binariks have the necessary expertise and can do everything for you.
Get started with FHIR with Binariks
Binariks is a healthcare software development company offering interoperability implementation , among other services. With our help, you can become FHIR-compliant and achieve better performance, care quality, and coordination within your organization.
We hire engineers proficient in healthcare software migration, optimization, and development. They can audit your existing systems to advise on achieving HL7 compliance or design compliant software from scratch. You choose the scope of involvement and collaboration model based on your business needs. It may be occasional consulting or a dedicated team 100% focused on your project.
Learn more about the projects we have completed for healthcare organizations and other customers here .
Final Thoughts
The choice between HL7 and FHIR is a responsible step for any healthcare organization as it involves long-lasting consequences. You won't be able to switch from one standard to another easily. Despite many things in common, they differ a lot.
FHIR is more innovative and adapted to connect mobile applications and smart devices. Other HL7 standards are focused on traditional healthcare systems. Thus, you may need to hire a third-party consultant to make the right choice to pick the best option.
FAQ
Share

