As of 2021, there have been at least 612 million documented cases of heart disease worldwide, which includes coronary artery disease, heart failure, stroke, valvular disease, and congenital heart disease. By 2050, the number of people living with heart disease will reach over 1.1 billion.
Since heart disease affects so many people, it is the most mundane health crisis that demands urgent action and effective management. AI in heart disease holds great potential for preventing, treating, and managing heart disease. AI can spot subtle patterns in medical imaging that doctors miss and interpret data instantly.
In general, AI in cardiology boosts speed, scale, and sensitivity of diagnosis and treatment, redefining what is possible in cardiovascular medicine.
In this article, we uncover the true potential of AI and cardiology working together using our case of improving an AI-based heart disease detection solution for a healthtech company specializing in non-invasive screening for heart diseases.
Why early detection of heart disease matters
Cardiovascular disease (CVD) is the leading cause of death globally. According to the World Health Organization, it accounts for nearly 18 million deaths per year, representing around 32% of all global deaths. CDC reports that in the US, 1 out of 5 deaths is caused by heart disease, and someone has a heart attack every 40 seconds. Most of the deaths (375,000 deaths annually ) are a result of coronary heart disease.
But heart disease does not just result in patient death; it is a cause of lifelong disability for people with conditions like congestive heart failure or structural heart diseases like valve disease and cardiomyopathies.
Delays in diagnosis often result in advanced-stage disease by the time symptoms appear. By then, patients are looking at a less effective, more expensive, invasive treatment with a poorer prognosis.
Using AI diagnostics holds a lot of potential, as symptom-based detection is too often too late to prevent serious consequences of conditions. There are many issues with traditional diagnostics today. Many heart conditions, like atherosclerosis or atrial fibrillation, remain silent until a major event occurs, so they remain undetected.
Moreover, more general symptoms of heart disease overlap with other conditions, making a diagnosis of heart disease overlooked until it becomes more advanced, especially for younger people who are not thought to have specific conditions. Traditional testing, like ECG and echocardiogram, can be improved with AI towards better interpretation.
Treating heart disease is also expensive. As per the American Heart Association, the direct and indirect cost of CVD is projected to reach .1 trillion by 2035.
Early detection of heart disease is critical because it can:
- Reduce the risk of heart attacks, strokes, and sudden cardiac death
- Allow for less invasive interventions than surgeries
- Improve prognosis and extend life expectancy
- Lower long-term healthcare costs
Early detection can really turn something potentially fatal into a manageable, low-risk condition with routine care. Let's imagine a 60-year-old with silent atrial fibrillation, who might never know they have it until a clot forms and causes a massive stroke. If an AI-powered ECG detects the condition early, it can be managed with blood thinners and medication, with the stroke entirely prevented.
Need AI expertise that delivers measurable efficiency and results?
How AI and ML assist in heart disease diagnosis
Using AI to diagnose heart disease and strokes is transforming how clinicians detect life-threatening conditions before symptoms appear. AI and ML assist in heart disease diagnosis by analyzing vast amounts of patient data to identify patterns and predict risk.
Here is how machine learning in cardiology works for different branches of the field:
1. ECG analysis (electrocardiograms)
AI models have demonstrated high precision in interpreting ECGs with pattern recognition. This enables early identification of:
- Atrial fibrillation (even in sinus rhythm)
- Ventricular arrhythmias
- Silent myocardial infarctions
- Subtle electrical patterns linked to structural heart disease
2. Echocardiography interpretation (EchoCG)
AI enhances the analysis of heart ultrasound data by:
- Automatically measuring cardiac function metrics (e.g., ejection fraction, wall motion)
- Detecting chamber enlargement or valve malfunctions
- Reducing subjectivity across different operators
This is especially impactful in under-resourced settings, where access to expert cardiologists may be limited, such as in rural hospitals.
3. Cardiac imaging (CT, MRI, OCT)
Advanced imaging techniques benefit significantly from AI support, which can:
- Detect early coronary artery disease by analyzing signs like plaque burden or arterial inflammation
- Pinpoint fibrosis, scarring, or myocarditis on cardiac MRIs
- Support real-time interventional decisions using OCT during stent placement
4. Risk prediction and stratification
AI models trained on large-scale health records and clinical data help:
- Estimate the 5-10 year risk of major events like heart attack, stroke, or sudden cardiac death
- Integrate lab results, lifestyle data, and even genetic predispositions for deeper personalization
- Prioritize patients for preventive care or therapy adjustments
- Support AI in chronic disease management
5. Wearables and continuous monitoring
AI-enabled wearables (e.g., AliveCor, CardiacSense) provide:
- 24/7 heart rhythm monitoring
- Real-time detection of arrhythmias or abnormal heart rates
- Alerts to clinicians or caregivers before symptoms escalate
6. Clinical decision support
AI systems act as intelligent assistants by:
- Suggesting diagnoses or next steps based on clinical guidelines
- Flagging lab or imaging anomalies
- Recommending triage or referral when certain thresholds are met
Key AI technologies used in cardiac health
Machine Learning (ML)
ML is the backbone of most AI systems in cardiology. These models learn from large datasets to detect patterns. They are used to classify health conditions and predict future risk.
Use cases:
- Predicting heart attack or stroke risk
- Classifying arrhythmias in ECG data
- Assessing ejection fraction from echocardiograms
Algorithms used:
- Decision trees / random forests are used for risk stratification and prediction, such as forecasting risk for 5–10 years of cardiovascular events.
- Support Vector Machines (SVMs) are used for binary classification tasks, such as detecting atrial fibrillation in ECG signals.
- Gradient Boosting (e.g., XGBoost) is for high-accuracy predictive modeling, such as assessing heart failure readmission risk.
- k-Nearest Neighbors (k-NN) are applied to pattern recognition, such as classifying ECG waveform abnormalities based on similarity to known disease profiles.
Deep learning
DL is a subset of ML that uses multi-layered neural networks. It handles high-dimensional data like medical images and time-series signals.
Use cases:
- Interpreting echocardiography, CT, or MRI scans
- Detecting structural heart abnormalities
- Analyzing ECGs and vectorcardiograms
Models used:
- Convolutional Neural Networks (CNNs) – for image-based diagnostics and ECG pattern recognition
- Recurrent Neural Networks (RNNs), especially LSTMs, are for analyzing time-dependent cardiac signals
- Autoencoders – for signal denoising and anomaly detection in biosignals
Natural Language Processing (NLP)
NLP allows AI systems to extract structured insights from unstructured clinical text.
Use cases:
- Identifying cardiovascular risk factors from EHRs
- Extracting outcomes from discharge summaries
- Automating diagnostic report generation
Techniques used:
- Named Entity Recognition (NER) – to identify diseases, medications, or symptoms in text
- Topic Modeling (e.g., LDA) – to cluster medical records by themes
- Transformer Models (e.g., BERT-based) – for high-context understanding and clinical summarization
Computer vision
CV enables the AI to analyze and interpret visual data. Mainly used in cardiac imaging.
Use cases:
- Segmenting heart chambers or vessels in CT/MRI scans
- Detecting valve defects, plaques, or calcification
- Guiding stent placement using real-time intravascular imaging (e.g., OCT)
Models used:
- CNNs – for standard image classification (normal vs abnormal)
- U-Nets – for medical image segmentation
- Vision Transformers (ViTs) – for advanced high-resolution analysis (contextual analysis of the image).
Reinforcement Learning (RL)
Reinforcement learning is a type of machine learning where an AI agent learns through trial and error for strategy optimization. So far, its use in cardiology has been experimental.
Use cases:
- Dynamic medication dosing based on real-time patient data
- Personalized treatment planning for chronic heart failure
- Optimizing long-term care strategies by learning from outcomes over time
Binariks case study: Early heart disease detection solution
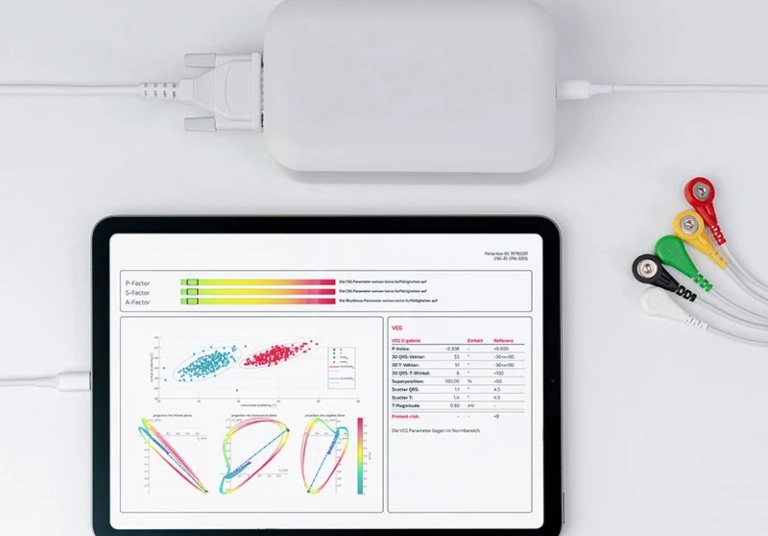
One of the most illustrative and successful cases of AI in cardiology that we worked with at Binariks is the project for a German health tech company focused on non-invasive, AI-powered early screening of heart disease.
Their flagship solution combines a proprietary 3D vector cardiography device with mobile and web applications to detect coronary and structural heart diseases before symptoms appear. The technology is a non-invasive diagnostic method that records electrical signals from the heart using 3D vector cardiography, which captures the spatial dynamics of cardiac activity.
Before collaborating with Binariks, they already had the prototype of their custom early heart-disease detection solution . The goal of our working together was to prepare the product for market entry.
Our client needed quality assurance to make sure its AI cardiology solution is reliable. Binariks prepared an end-to-end quality assurance process that also considered regulatory compliance.
We implemented test validation workflows and continuous improvement checkpoints, and decided to transition the platform to a more cost-efficient Raspberry Pi–based architecture with Python.
As a result:
- Achieved 80% test case coverage for product reliability
- Stabilized cross-platform performance in clinical and mobile settings
- Ensured integration between AI models and hardware under real-world conditions
- Strengthened readiness for medical certification and regulatory review
With our help, our client was ready to expand its AI-based screening tool into broader markets with a clinically viable product.
Build compliant healthcare technologies that deliver real clinical impact
Benefits of using AI in heart disease detection
1. Earlier detection of silent or asymptomatic disease
AI in cardiology can uncover hidden signs of heart dysfunction before symptoms appear.
Example: Researchers at the Mayo Clinic trained a deep learning model on routine 12-lead ECGs to detect asymptomatic left ventricular dysfunction, achieving an AUC of 0.93. This condition is often missed in regular exams.
2. Greater diagnostic accuracy
AI models can match or even outperform experienced clinicians when interpreting complex data like ECGs and echocardiograms in heart disease detection using AI.
Example: Stanford's EchoNet-Dynamic model predicted ejection fraction from echocardiograms with similar accuracy to board-certified cardiologists, achieving Pearson r > 0.95.
3. Faster diagnosis and clinical efficiency
AI reduces the time required for data interpretation and enables clinicians to focus on critical decisions.
Example: At Mayo Clinic, AI-enhanced ECG screenings flag potential heart dysfunction in seconds.
4. Risk stratification & predictive modeling
Machine learning helps forecast the likelihood of future cardiac events by analyzing large-scale patient datasets.
Example: ML models trained on the UK Biobank population outperformed traditional tools like the Framingham Risk Score in predicting 5-year cardiovascular mortality.
5. Scalability and accessibility
AI tools enable diagnostics in remote or resource-limited settings.
Example: Our client's AI-based vectorcardiography system offers non-invasive screening via web and mobile tools, without the need for ultrasound or CT/MRI.
6. Reduced healthcare costs
AI helps reduce the cost of care by identifying issues early and avoiding unnecessary imaging or hospitalizations. Preventing even one heart failure admission, which can cost ~$20,000 in the US, through early AI-based detection translates to significant cost savings at scale.
Example: A Mayo Clinic–led study of approximately 22,000 outpatients showed that AI‑guided ECG screening for low ejection fraction (EF) that triggers echocardiography only when needed had a cost‑effectiveness ratio of $27,858 per QALY, and just $1,651 per QALY when limited to outpatient settings.
7. Continuous learning and real-world validation
Unlike static diagnostic protocols, AI systems improve with more data and can generalize across institutions using federated learning.
Example: Our client's cardiograph was validated in over 30 clinical centers across Europe, allowing the AI to perform reliably on diverse patient populations. Diagnostic performance is expected to improve with continuous usage via model fine-tuning and retraining.
Possible challenges
Here are the common industry-wide challenges for AI in cardiovascular disease, and ways to manage them. This also includes challenges we encountered when working on AI in heart disease solutions for our client.
1. Regulatory compliance & certification
Challenge:
Medical AI tools must meet strict regulatory standards (e.g., FDA, CE under MDR). In our case, the AI-driven heart screening platform needed to align with European MDR regulations.
Solution:
Establish QA and documentation processes aligned with medical software standards. This includes:
- Comprehensive test case coverage
- Documented validation and verification steps
- Regular internal audits and compliance checkpoints
These practices accelerate certification readiness and support future audits or updates.
2. Hardware–software integration
Challenge:
AI models often need to run on embedded systems or proprietary hardware, which can create performance or compatibility issues, especially in mobile or low-power settings. The AI in heart disease detection solution we worked on had to run on a proprietary cardiograph device used in varied clinical settings, including low-resource environments.
Solution:
Optimize hardware-software compatibility early in development by:
- Choosing efficient hardware platforms (e.g., Raspberry Pi, Jetson Nano). Within our project, we adopted a Raspberry Pi–based architecture because it provided the right balance of processing power and low cost. It made it possible to run AI diagnostics directly on the device in clinics.
- Leveraging lightweight frameworks and optimized runtimes
- Closely testing the full AI pipeline under realistic clinical conditions
3. Cross-platform compatibility
Challenge:
Diagnostic apps must work seamlessly across different devices and operating systems in clinical settings. The diagnostic platform we worked on included web and mobile apps on both Android and iOS.
Solution:
Implement end-to-end QA for:
- Android and iOS mobile platforms
- Major web browsers and operating systems
- Different screen sizes and device types
- Combined automated and manual testing ensures consistency and usability across environments.
4. Data sensitivity & privacy
Challenge:
Medical AI systems must protect patient data and comply with regulations like GDPR, HIPAA, or regional equivalents.
Solution:
Ensure all testing and development processes:
- Use anonymized or synthetic patient data where possible
- Align with encryption and access control standards
- Support audit trails and secure logging for traceability
Although our focus with the mentioned project was QA, we ensured that data handling in testing environments followed best practices. This included anonymizing patient inputs during simulation and aligning with security protocols required for certification.
5. AI robustness in real-world conditions
Challenge:
AI systems that perform well in controlled lab settings may underperform with real-world variability.
Solution:
Conduct robust validation by:
- Testing under variable and degraded input conditions
- Including edge-case scenarios in model evaluation
- Incorporating human-in-the-loop feedback during pilot phases
With our client, we ran stress and edge-case testing to validate how the AI system responded under variable input quality (e.g., signal noise from patient movement).
Why choose Binariks as your AI development partner
We recognize that cardiological AI goes beyond simple algorithms; it is about saving lives.
As an AI development partner for cargological projects, Binariks combines deep clinical knowledge with regulatory expertise to build AI solutions that actually work in real healthcare environments.
We provide:
- Proven AI & ML expertise from predictive modeling to diagnostic automation
- Strong healthtech expertise. Our portfolio includes over 60 projects related to AI decision support tools, RPM platforms, telehealth, embedded software, EHR integration, medical imaging, custom early heart-disease detection, data analysis, hospital management, and more
- DTx consulting and development services
- End-to-end healthcare development services with medical compliance
- Full-cycle development & QA
- Building for scalability and cross-platform implementation
Future of AI in cardiology and final thoughts
Artificial intelligence in heart disease continues to shape the future of cardiology. As heart disease continues to be the world's leading cause of death, healthcare systems are actively seeking smarter, faster, and more scalable diagnostic tools. AI is no longer experimental; it's becoming an essential part of routine cardiology.
The key trends that drive the growth of artificial intelligence in cardiology are:
- Widespread clinical adoption of automated tools for ECG and imaging
- Integration with wearables
- More and more AI-based cardiac solutions are receiving CE and FDA clearances.
- Individualized risk assessment for preventative care enabled by AI.
The FDA has cleared over 1,000 AI medical algorithms, with cardiology as the second-largest specialty. This means that we are about to see more and more technologies hit the market in the future, like AI‑enhanced Digital stethoscopes for heart murmur diagnosis, Tempus ECG-Low EF and ECG-AF Algorithms for low ejection fraction, and an aortic stenosis AI‑ECG algorithm.
A specialized partner like Binariks brings healthcare expertise, technical depth, and regulatory experience together for a product ready for the clinic.
Contact us if you want to build AI for heart disease detection or treatment.
Share

