Have you ever wondered how healthcare providers across different systems and locations can seamlessly share and understand your medical records, ensuring you receive consistent and informed care wherever you go?
On the one hand, there is FHIR, which addresses how to exchange data - providing the framework and standards for how this data is structured. In this article, we will focus on USCDI (United States Core Data for Interoperability), which specifies the what of data exchange - the actual set of standardized data elements and classes (like patient demographics, lab results, medication lists) that need to be shared across different healthcare systems.
The article contains a USCDI FHIR comparison, details on how to implement USCDI with FHIR, and uses cases of such implementation.
Introduction to USCDI
The United States Core Data for Interoperability (USCDI) is a standardized set of health data classes and elements for nationwide, interoperable health information exchange. At its core, USCDI is a content standard that specifies what data should be included in health records for interoperability.
USCDI is a standard that mandates and obligates healthcare systems to transmit or receive data according to a specific set of rules. The essence of these rules is the inclusion of a minimum set of information within particular data types. For instance, the data type 'Patient' should contain a certain set of fields per USCDI standards (like FirstName, LastName, MiddleName, etc.).
USCDI standard makes it easy for healthcare organizations to share data. It was developed by the Office of the National Coordinator for Health Information Technology (ONC), a part of the US Department of Health and Human Services.
The rationale behind developing USCDI was to standardize data exchange between healthcare systems. Before such standardization, there were scenarios where one system might consider certain data mandatory while another did not.
Standardization is crucial as it allows healthcare organizations to communicate. Electronic health records (EHRs) and other health IT systems can exchange information seamlessly with standardized data. This leads to quality improvements in patient care as healthcare professionals access up-to-date patient information, and patients can receive timely care at any healthcare organization.
Key components of USCDI
The critical components of the USCDI standard are the data elements. One can find the list of USCDI data elements on the United States Core Data for Interoperability (USCDI) website. Examples include:
- Patient demographics: basic information about the patient, such as name, sex, date of birth, race, ethnicity, and preferred language.
Elements: Name, Sex, Date of Birth, Race, Ethnicity, Preferred Language, etc.
- Clinical notes: These are various types of notes generated by healthcare providers. This may include consultation notes, discharge summary notes, history and physical notes, and procedure notes.
Elements: Consultation Notes, Discharge Summary Notes, History and Physical Notes, Procedure Notes, Progress Notes, etc.
- Medications: Information about medicines prescribed to or taken by a patient.
Elements: Medication Name, Dosage, Frequency, Route, etc.
- Allergies and intolerances: Details about any allergies or intolerances a patient may have, including the substance and reaction.
Elements: Substance, Reaction, Severity, etc.
- Lab tests and results: Includes laboratory test orders and results.
Elements: Test Name, Result, Date, etc.
- Vital signs: Basic physiological measurements such as blood pressure, heart rate, body temperature, respiratory rate, and BMI.
Elements: Blood Pressure, Heart Rate, Body Temperature, Respiratory Rate, BMI, etc.
- Problems: Information about health conditions or issues a patient is experiencing or has experienced.
Elements: Health Conditions, Diagnosis, etc.
- Immunizations: Records of vaccines a patient has received.
Elements: Vaccine Type, Date, Dose, etc.
- Procedures: Details about medical procedures the patient has undergone.
Elements: Procedure Type, Date, Provider, etc.
Other USCDI data elements include but are not limited to assessment and treatment plan, care team members, goals, smoking status, and diagnostic images.
Versions
As of 2023, the USCDI standard has four versions. The United States Core Data for Interoperability (USCDI) evolves, with each version expanding and refining the standardized data set for health information exchange.
- USCDI V1 is the first standard that established the foundational data classes and elements for interoperability through the ONC Cures Act Final Rule. It was established in 2020.
- USCDI V2 introduced new USCDI data elements, such as health insurance data information and pediatric data signs.
- USCDI V3 introduces additional USCDI data elements.
- USCDI V4 is the latest standard, introducing 20 additional USCDI data elements.
Levels
Levels in the context of USCDI standards refer to the stages of data class inclusion. These include Draft Standard for Trial Use (DSTU) and Final Standard. DSTU includes data classes and elements proposed for inclusion in the USCDI. They go through trial and feedback before transforming into Final Standard, included in the next version of USCDI.
How to become FHIR-compliant
FHIR implementation guide

Difference between USCDI and HL7
To understand the difference between USCDI and HL7, focusing on USCDI vs FHIR is essential, as HL7 is one of the standards of FHIR. You can read more on FHIR vs. HL7 .
USCDI and FHIR often work together in healthcare data exchange, but they differ. FHIR, as an interoperability standard, is primarily concerned with the technical aspects of healthcare data exchange, answering how data should be transmitted. On the other hand, the USCDI standard focuses on the content of the data being exchanged, specifying what specific data should be transmitted.
While FHIR provides the framework and protocols for how healthcare data is structured and exchanged between systems, USCDI defines the specific types of data (like patient demographics, lab results, clinical notes, etc.) that must be included in these exchanges. This distinction is crucial for ensuring that healthcare data is transmitted efficiently and securely (thanks to FHIR) and is meaningful and valuable for healthcare providers (as ensured by USCDI). This synergy between FHIR and USCDI is critical to achieving effective interoperability in healthcare.
Regarding USCDI and HL7 precisely, USCDI aligns with the FHIR HL7 data format and is intentionally similar to it. When making new additions to USCDI standards, OSC considers HL7 data elements.
USCDI is developed and maintained by the Office of the National Coordinator for Health Information Technology (ONC), a federal entity within the US Department of Health and Human Services. In contrast, HL7 is developed by not-for-profit Health Level Seven International. USCDI is designed for the US healthcare system, while the HL7 standard is used worldwide.
USCDI and FHIR integration
USCDI and FHIR are integrated through FHIR profiles. A profile is a set of rules an FHIR server expects and works with at its API level. The FHIR US Core is an example of such a profile. USCDI and US Core are integrated on a common basis.
US Core is a collection of rules defining how data should be structured and exchanged per the USCDI standards. In other words, the FHIR US Core profiles ensure that an FHIR API handles and exchanges data in a way that aligns with the data types and structures defined by USCDI. US Core data for interoperability represents a specific subset of FHIR resources designed for interoperability. US Core allows data exchange facilitated by USCDI.
FHIR APIs can access and exchange data defined by the USCDI. This makes it easier for healthcare providers to access critical patient information in a consistent format, irrespective of the underlying EHR systems.
The FHIR US Core essentially adapts the broader FHIR standard to the specific context of the US healthcare system. It bridges FHIR's technical capabilities with the data content requirements of USCDI, ensuring that healthcare data is interoperable in a manner that is compliant with US standards.
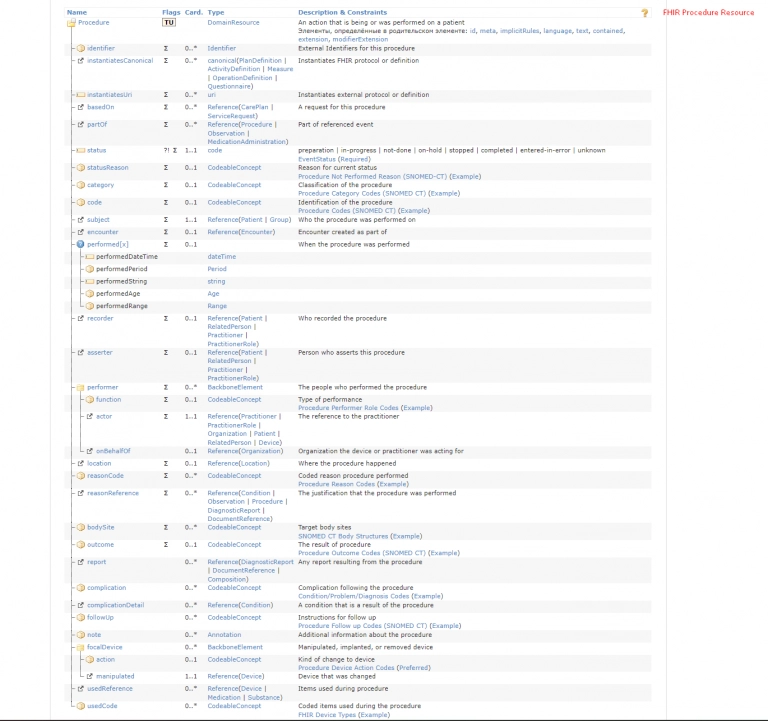
An example Of US Core FHIR Procedure resource
Benefits and implications
Using USDCI and FHIR together for seamless data exchange has a lot of benefits for healthcare professionals, patients, and the healthcare system in general. Let's review the most essential ones.
Improved data sharing
USCDI FHIR facilitates seamless and efficient sharing of health information across different health IT systems and applications. This integration also enables real-time access to patient data, which is crucial in urgent care scenarios.
Enhanced patient care
USCDI FHIR integration ensures that comprehensive and critical patient information is readily available to healthcare providers, leading to better-informed clinical decisions. Clinicians can access more complete patient records, including historical data, essential for accurate diagnosis and treatment planning.
Increased effectiveness of the healthcare system
USCDI FHIR integration is helpful for the healthcare system as a whole:
- Streamlined data sharing helps reduce administrative burdens, allowing healthcare providers to allocate more resources to patient care.
- Cost savings can occur through minimizing errors and redundant tests.
- The system becomes more agile and responsive to changes in healthcare demands, whether due to public health emergencies or shifts in population health needs.
Use cases and examples
Here are some of the most common examples of how USCDI FHIR dual implementation:
- A unified patient health record system that leverages FHIR to structure and exchange data defined by USCDI.
- Emergency departments accessing critical patient information in real-time using FHIR APIs, with data adhering to ONC USCDI standards.
- Patients accessing their health records through mobile or web applications that utilize FHIR for data retrieval, formatted according to USCDI.
- Integration of continuous monitoring devices (like glucose monitors for diabetes) with EHRs using FHIR. The data shared aligns with USCDI elements, such as lab results and medications.
Harness the full potential of healthcare interoperability with Binariks
Final thoughts
The United States Core Data for Interoperability (USCDI) represents a significant advancement in healthcare standardization. In the future, we can expect even more interoperability among different healthcare systems as USCDI standards progressively incorporate more elements. At Binariks, we can address the critical steps of USCDI FHIR integration, such as:
- Data mapping of USCDI data elements
- FHIR-compliant APIs integration
- Testing and validation
- Maintenance
Share

