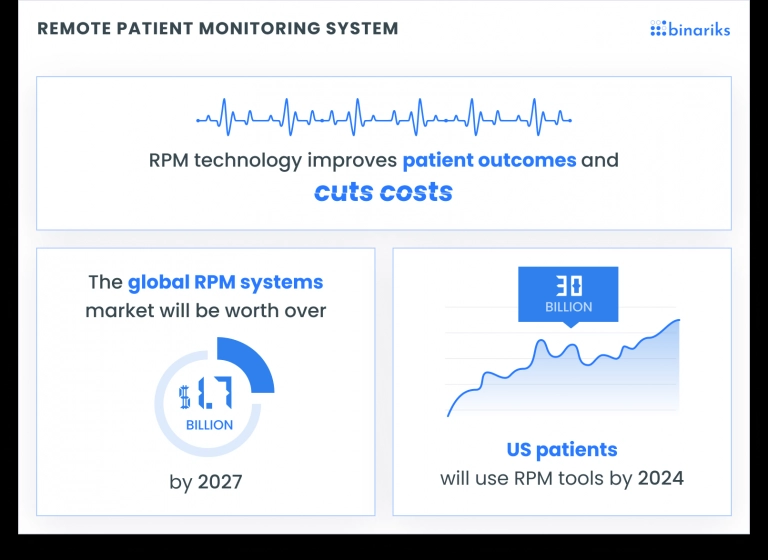
According to Insider Intelligence, nearly 70.6 million US patients, or 26.2% of the population, will use RPM tools by 2025. Remote Patient Monitoring (RPM) has revolutionized healthcare by allowing providers to track patients' health conditions remotely.
You can gather real-time data on vital signs, symptoms, and well-being through wearable devices and mobile apps. But, to ensure proper payment, it is crucial to navigate the remote patient monitoring reimbursement process.
RPM offers many benefits, like reducing hospital readmissions and improving patient engagement. But still, the complexities of reimbursement policies and procedures pose challenges.
This article will help you maximize patient care and streamline billing procedures. Here are our key considerations, recommendations, and best practices on RPM reimbursement for healthcare providers and managers.
Understanding RPM reimbursement
Healthcare professionals should understand the inside process for proper remote patient monitoring reimbursement. It is guided by specific codes and instructions that provide a framework for accurate billing and reporting.
Private insurance companies' coverage options and payment models may differ from Medicare. It is crucial to know it for maximizing reimbursements for remote patient monitoring (RPM).
Medicare reimbursement for RPM
Medicare, administered by CMS, provides reimbursement for RPM services based on specific criteria. To qualify, healthcare providers must meet certain requirements. For example, using designated payment codes and maintaining proper documentation. These codes capture the complexity and duration of RPM services, ensuring precise reimbursement.
Thorough documentation of patient interactions, device usage, and care management processes is essential to substantiate services and support reimbursement.
Private payer reimbursement
Beyond Medicare, private insurance companies provide reimbursement for RPM services, with varying coverage options and payment models. Healthcare providers must familiarize themselves with individual insurance company policies.
For instance, there can be specific requirements or limitations regarding eligible conditions or patients for reimbursement. Providers may also need to follow distinct documentation requirements or prior authorization processes.
Private payers may offer different reimbursement models, such as bundled payments or value-based reimbursement, which may require additional reporting or outcome measurements.
Staying informed and adhering to documentation requirements enables healthcare providers to optimize reimbursement while delivering comprehensive RPM care.
Examples of the CPT codes for RPM reimbursement
Here are some examples of the CPT Codes used in remote patient monitoring reimbursement.
- CPT Code 99453: This code is used for billing for the initial setup and patient education related to RPM services. It covers the time spent on the initial device supply, instructions on proper use, and patient onboarding.
- CPT Code 99454: This code is used for billing for the supply and monitoring of a patient's physiological data. It includes the initial device supply and daily recording, transmission, and receipt of patient-generated health data.
- CPT Code 99457: This code is used for billing for the first 20 minutes of clinical staff time spent on interactive communication with the patient or caregiver to manage RPM data, interpret results, and subsequent treatment adjustments.
- CPT Code 99458: This code is an add-on code to CPT Code 99457 and is used for billing for each additional 20 minutes of clinical staff time spent on interactive communication beyond the initial 20 minutes.
- CPT Code 99473: This code is used for billing for the initial set-up and patient education related to self-measured blood pressure monitoring. It covers the time spent on device supply, instructions on proper use, and patient training.
- CPT Code 99474: This code is used for billing for the supply and monitoring of self-measured blood pressure data. It includes providing a validated device, training on proper use, and reviewing and interpreting patient-generated blood pressure readings.
- CPT Code 99490: This code is used for billing for chronic care management services, which may include RPM. It covers at least 20 minutes of clinical staff time per calendar month spent on care coordination, medication management, and communication with other healthcare professionals involved in the patient's care.
Remember always to check your reimbursement for rpm codes. It's important to refer to the most up-to-date coding guidelines provided by CMS and professional coding organizations for accurate billing and reimbursement practices.
Want to become FHIR-compliant?
Learn about best practices of FHIR implementation

Ensuring RPM reimbursement
Effective remote patient monitoring reimbursement for 2023 requires healthcare providers to navigate various aspects.
This section will explore key considerations, including compliance with criteria, proper documentation practices, accurate coding and billing procedures, proactive communication with payers, staff training and education, quality assurance, and performance monitoring.
Compliance with reimbursement criteria
To ensure successful RPM reimbursement, healthcare providers must comply with the criteria established by government agencies and private payers. This involves updating the eligibility requirements, service limitations, and documentation guidelines.
Don't forget about regular reviews and adjustments to align RPM services with the reimbursement guidelines.
Proper documentation
Comprehensive and accurate documentation is crucial for RPM reimbursement. Healthcare providers should establish robust documentation practices that capture all relevant information, including patient interactions, care management activities, and treatment adjustments based on collected health data.
Thorough documentation supports the medical necessity of RPM services and facilitates efficient billing processes.
Coding and billing considerations
Accurate coding and billing practices will help in maximizing reimbursement and minimizing errors. You should use appropriate CPT codes that accurately reflect the RPM services, including initial setup, device supply, monitoring, and interactive communication. Staying updated with coding guidelines, modifiers, and bundling rules specific to RPM services is a must for accurate billing.
Communication with payers
Proactive communication with payers will help to smooth the reimbursement process. Healthcare providers should regularly talk with payers to understand specific requirements, coverage policies, and documentation expectations for RPM services.
Effective communication helps clarify reimbursement policies, resolve inquiries or concerns, and build strong provider-payer relationships.
Best practices for RPM reimbursement
A recent survey of providers offering RPM services indicated that there are some challenges impacting RPM prescription behavior.

In this section, we will explore best practices like staff education, tech and data integration, audit readiness, performance monitoring, and outcome measurement.
By following these remote patient monitoring reimbursement tips, healthcare providers can optimize outcomes, improve operational efficiency, and deliver high-quality care.
Staff education and training
Healthcare providers should offer comprehensive training programs to their staff members involved in RPM services, including physicians, nurses, and administrative personnel.
Training should cover topics such as RPM reimbursement policies, proper documentation practices, accurate coding and billing procedures, and effective communication with payers. Ongoing education keeps the staff updated with the latest guidelines, equipping them with the knowledge and skills necessary for compliant and efficient reimbursement processes.
Technology and data integration
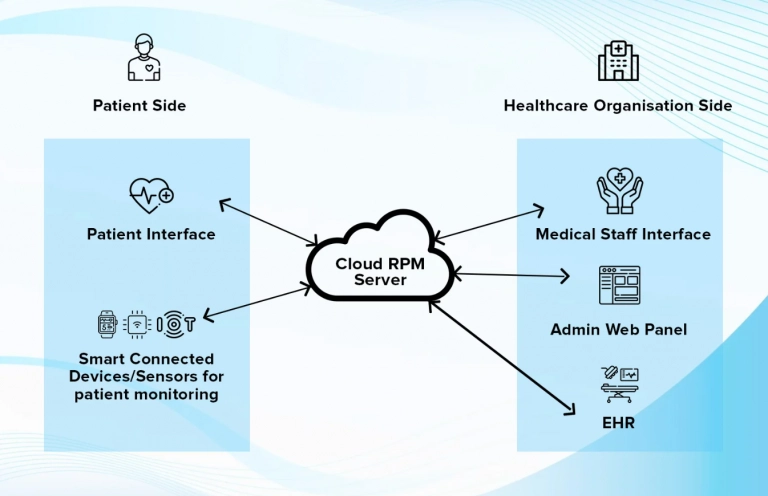
Leveraging appropriate technology solutions and integrating data effectively are essential for maximizing RPM reimbursement.
Find RPM platforms that facilitate seamless data collection, analysis, and reporting. These platforms should integrate with electronic health record (EHR) systems to streamline documentation and ensure accurate patient data capture.
By leveraging technology and integrating data across systems, you can improve the efficiency of reimbursement workflows, enhance data accuracy, and support the medical necessity of RPM services.
Compliance and audit readiness
RPM reimbursement also requires compliance and audit readiness to be maintained. Establishing robust compliance programs to encompass ongoing monitoring, internal audits, and adherence to regulatory guidelines is important.
Regular reviews of documentation, coding, and billing practices can identify areas of improvement and help mitigate compliance risks. Such an approach will help minimize reimbursement delays, denials, and potential penalties.
Performance metrics and outcome measurement
Implementing performance metrics and outcome measurement strategies allows healthcare providers to demonstrate the effectiveness and value of RPM services, thereby supporting successful reimbursement.
By tracking key performance indicators, such as patient engagement rates, health outcomes, and cost savings, providers can showcase the impact of RPM on patient care and overall healthcare outcomes. Robust data analysis and reporting can help quantify the benefits of RPM, enhancing the justification for reimbursement and fostering collaboration with payers.
Quality assurance and performance monitoring
Implementing quality assurance measures and performance monitoring systems helps maintain high standards in RPM reimbursement. Regular evaluations of documentation accuracy and completeness, coding and billing audits, and monitoring the timeliness of reimbursement submissions are essential.
Continuous monitoring enables providers to identify areas for improvement, address issues promptly, and optimize RPM reimbursement outcomes.
Continuous quality improvement
Emphasizing continuous quality improvement is vital for successful RPM reimbursement. Healthcare providers should establish quality improvement programs that promote regular reviews of processes, documentation, and reimbursement outcomes.
By identifying opportunities for enhancement and implementing evidence-based practices, providers can optimize the quality and efficiency of their RPM services. Continuous quality improvement efforts demonstrate a commitment to delivering high-quality care and can contribute to improved reimbursement outcomes.
Maximizing RPM reimbursement with Binariks solutions
Partnering with the right software development company is crucial for successful remote patient monitoring . Binariks specializes in creating cutting-edge solutions that seamlessly combine virtual and traditional care, allowing healthcare providers to optimize medical resources and deliver high-quality care remotely.
We offer comprehensive remote patient monitoring software development services, including seamless integration with Electronic Health Records (EHR) systems. Our custom RPM applications enable secure access to patient medical history, medication management, and real-time treatment progress monitoring.
Choosing Binariks as your remote patient monitoring development partner means gaining access to a team of experienced professionals with in-depth knowledge and expertise in developing top-notch RPM solutions.
We guarantee transparent communication, real-time cost estimates, and the ability to scale teams based on your organization's needs. Our software engineers, solution architects, business analysts, and quality assurance professionals ensure the delivery of world-class, HIPAA-compliant patient monitoring software.
Build compliant and secure RPM apps with healthcare software engineering experts
Final thoughts
We hope this short guide helped you explore key RPM reimbursement aspects. Remember that best practices such as compliance with reimbursement criteria, proper documentation, coding and billing considerations, communication with payers, staff education and training, and technology integration are essential for successful RPM reimbursement.
By understanding the complexities of RPM reimbursement and implementing recommended strategies, you can navigate the reimbursement sphere effectively. Compliance, documentation, coding accuracy, and clear communication with payers ensure appropriate payment for RPM services.
Investing in staff education, training, and technology integration also contributes to successful reimbursement, helping you deliver high-quality care, improve patient outcomes, and adapt to the evolving healthcare landscape.
FAQ
Share

