Keeping tabs on patients outside the hospital has never been more critical. With staff stretched thin, chronic illnesses on the rise, and readmission penalties stacking up, healthcare teams need a better way to stay connected. This is where remote patient monitoring devices come in. They bring care to patients wherever they are by tracking vitals and sending real-time updates directly to care teams.
And the numbers back it up. According to Fortune Business Insights , the global market for RPM devices is expected to soar from $50.39 billion in 2024 to $203.68 billion by 2032, growing at a CAGR of 19.1%. North America currently leads the charge, holding nearly 48% of the market.
This surge is driven by rising chronic conditions like hypertension, diabetes, and COPD, as well as better reimbursement policies and faster innovation in sensor technology.
In this article, we'll break down what RPM means in practice, which devices matter most, and how they're helping reshape care across hospitals, homes, and everything in between.
Here's what you'll take away:
- How RPM benefits both patients and providers
- The key categories of monitoring devices on the market
- 10 real-world examples of RPM in action
- What to look for when choosing an RPM solution
- How Binariks helps build and scale RPM systems
If you're exploring RPM for your organization or want to see how it fits into your digital health roadmap, read on. The right tools might already be out there, and we'll show you how to find them.
Benefits of remote monitoring in healthcare
Remote patient monitoring devices are improving how care is delivered, not by replacing in-person visits, but by filling the gaps between them. These tools make healthcare more continuous, more connected, and more responsive to each patient’s needs.
For patients: More confidence and control
RPM devices give patients more than numbers – they give peace of mind and real involvement in their care.
- Ongoing support from home. No need to wait for the next appointment. Patients can monitor their vitals daily and get alerts when something's off.
- Fewer hospital visits. With early detection, many issues are caught before they become emergencies, reducing ER trips or readmissions.
- Better understanding of their health. Seeing daily trends from health monitoring devices helps patients take action earlier and stick to their treatment plans.
For doctors: Real-time data, better care
Clinicians get a clearer, more complete picture of each patient's condition, without extra paperwork or second-guessing.
- Accurate, real-time updates. Instead of relying on memory or incomplete data, doctors get a live feed of patient vitals and trends.
- Tailored treatment plans. Patterns captured by remote monitoring help doctors adjust care based on what's actually working, not just what should.
- Faster communication. With shared data dashboards, care teams can coordinate more smoothly and keep everyone aligned.
For healthcare organizations: Efficiency that scales
Hospitals, clinics, and digital health platforms use RPM to improve care delivery, cut costs, and manage growing demand.
- Lower operating costs. Remote patient monitoring helps prevent unnecessary admissions, thus saving resources and reducing strain on staff.
- Smarter use of time and personnel. Thanks to real-time alerts and centralized data systems, teams can focus attention where needed most.
- Stronger patient engagement. When patients feel supported and informed, satisfaction scores rise – and so does long-term loyalty to the provider.
Types of RPM devices
There's no one-size-fits-all when it comes to remote care. Each RPM device is designed to track specific health conditions or metrics. Below is a breakdown of the main categories of medical monitoring devices used today.
| Type of Device | Tracked Metrics | Use Cases | Target Patients |
| Vital signs monitors | Blood pressure, heart rate, temperature | General health tracking, hypertension management, post-surgery recovery | Older adults, post-op patients |
| Glucose monitors | Blood glucose (real-time or periodic readings) | Continuous or spot-check glucose monitoring for diabetes | Type 1 & Type 2 diabetics |
| Pulse oximeters | Blood oxygen saturation, pulse rate | Monitoring respiratory issues like asthma, COPD, or COVID-19 | Pulmonary patients, post-COVID cases |
| Smart weight scales | Body weight, BMI, fluid retention | Managing congestive heart failure, obesity, or kidney-related conditions | Cardiac, renal, or bariatric patients |
| Wearable health devices | Physical activity, sleep, heart rate variability | Lifestyle monitoring, post-discharge recovery, fall detection | At-risk seniors, rehab patients |
| ECG/EKG monitors | Electrical heart activity, irregular rhythms | Detecting arrhythmias, monitoring cardiac patients between visits | Cardiology patients |
| Multi-parameter devices | Several vitals: BP, HR, SpO2, temp in one unit | Remote monitoring programs, home care setups | Broad home-based care for high-risk or polymorbid patients |
Each health monitor device plays a specific role in delivering timely insights and guiding medical decisions. In the next section, we'll walk through five real-world examples of RPM devices in action.
10 examples of remote patient monitoring (RPM) devices
From chronic disease to post-surgical recovery, remote patient monitoring relies on specialized tools that deliver real-time, high-quality data to care teams. Below are ten essential devices used in modern remote patient monitoring systems, explained in depth.
Blood pressure monitors
Used in nearly every chronic care RPM program, home-based blood pressure monitors help track hypertension, heart failure, and post-operative stability. These devices use digital cuffs to take systolic and diastolic readings, which are then automatically sent to care teams through mobile apps or cloud platforms.
As mentioned in The Times , Scotland's Connect Me program cut 400,000 annual GP visits by giving patients at-home BP cuffs, saving the NHS over £15 million and proving that a well-designed remote health monitoring system can have a measurable population-level impact.
Key functions:
- Detect early signs of hypertension or hypotension;
- Reduce hospital visits through routine home checks;
- Sync with RPM dashboards for trend analysis.

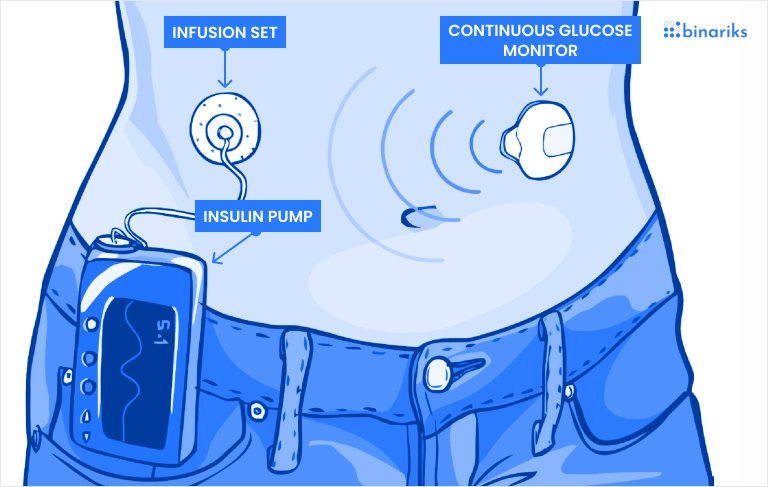
Glucometers, continuous glucose monitors (CGMs)
Whether a handheld glucometer or a sensor-based CGM, blood glucose monitoring is the backbone of diabetes care. Devices like Dexcom G6 and Abbott FreeStyle Libre send real-time blood sugar data directly to apps and dashboards. These remote patient monitoring systems support smarter insulin use, dietary awareness, and safer management of Type 1 and 2 diabetes.
A recent study found that 65-70% of Americans would join an RPM program to monitor vitals like glucose, and 80% said it would positively impact their care delivery.
Common features:
- Real-time glucose tracking and alerts;
- Retrospective data analysis for insulin adjustments;
- Integration with insulin pumps or telehealth apps.
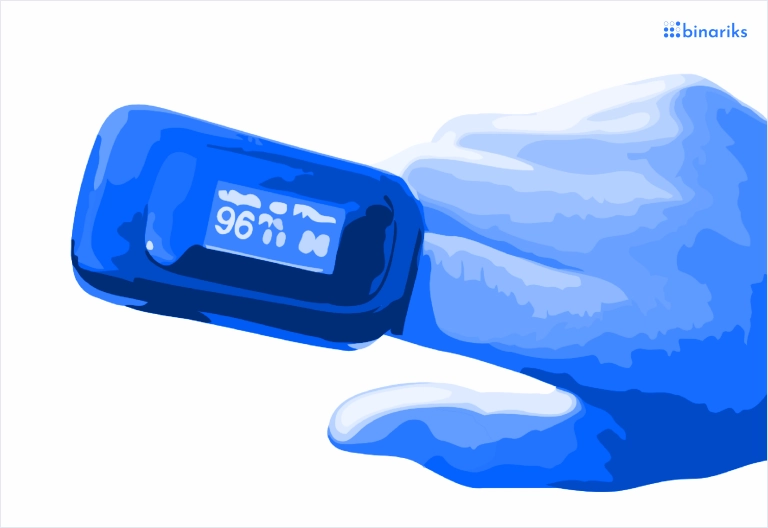
Pulse oximeters
These small, finger-clip sensors became vital during the COVID-19 pandemic and remain a staple for anyone with respiratory risks. Pulse oximeters measure SpO₂ and pulse rate, offering immediate data that feeds into broader remote patient monitoring technology platforms. They're ideal for COPD, asthma, long COVID, and sleep apnea.
Modern versions sync automatically with apps and alert providers when oxygen drops below safe levels. In multi-device setups, oximeters are often used alongside thermometers or smart inhalers.
Used for:
- Real-time respiratory distress alerts;
- Overnight oxygen monitoring;
- Early detection of post-op complications.
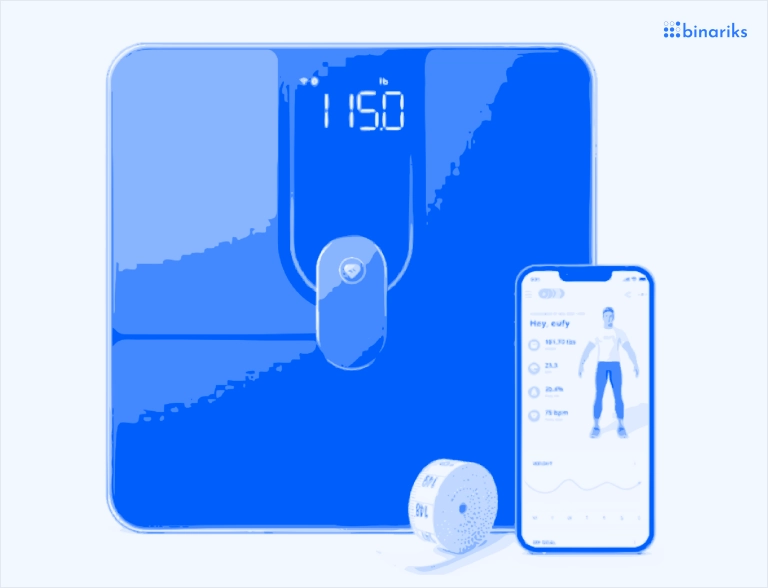
Smart weight scales
Subtle weight fluctuations can signal serious issues, especially in heart failure or kidney disease. That's where connected weight scales come in. These remote patient monitoring technologies detect even small changes in water retention or BMI, triggering timely intervention.
Patients weigh themselves daily, and data is sent directly to cardiology or nephrology care teams. Some scales also estimate body composition or muscle mass to support broader recovery goals.
Features include:
- Auto-sync to RPM apps and EMRs;
- Alerts for rapid weight gain (heart failure);
- Medication side effect monitoring (e.g., steroids).
Wearable fitness trackers
From Apple Watch to Garmin to Fitbit, wearable health devices track sleep cycles, HR variability, blood oxygen, and more.
These tools have found their way into formal clinical programs for rehab, post-op recovery, and elderly care. As part of continuous health monitoring, they fill in gaps between medical touchpoints with constant lifestyle data.
Recent research published in the IEEE Journal of Biomedical and Health Informatics shows how wearables, combined with deep learning and 5G, can monitor and predict changes in vital signs with 96.5% accuracy, and just 14.4 milliseconds of latency.
The proposed CNN-LSTM architecture outperformed existing solutions in speed and precision, enabling real-time alerts for deteriorating conditions. This demonstrates how wearables are becoming essential clinical-grade telemonitoring devices, not just fitness tools.
Tracked metrics:
- Daily step count and movement;
- Sleep quality and duration;
- Resting heart rate and HR variability trends.
ECG/EKG monitoring devices
These devices capture electrical heart activity to detect rhythm abnormalities, such as atrial fibrillation, PVCs, or prolonged QT intervals. Worn as patches, chest straps, or smart wearables, ECG monitors offer essential insights into cardiac performance over time. They're especially useful post-MI or in stroke risk management as part of personal health monitoring programs.
Some devices automatically notify care teams if a patient experiences arrhythmia or bradycardia, enabling rapid triage.
Key capabilities:
- Beat-by-beat tracking of cardiac rhythm;
- Remote detection of AFib and other anomalies;
- Integration with cardiologist RPM platforms.
Smart thermometers
Temperature data can signal infection, inflammation, or immune response changes. Smart thermometers used in telemonitoring devices connect with care platforms to provide real-time insights. They are often used in pediatric RPM, cancer recovery, or post-surgical care to track signs of fever or sepsis.
Smart thermometers are often bundled with multi-symptom checkers or caregiver alerts for better oversight of at-risk populations.
Common applications:
- Monitoring neutropenic patients (e.g., after chemo);
- Detecting post-op infections early;
- Daily vitals in elderly care programs.
Respiratory monitoring devices
These include chest-worn sensors, connected spirometers, and even AI-enhanced breath analyzers. Used in post-COVID clinics, COPD programs, and pediatric asthma management, they help track respiratory rate, lung function, or carbon dioxide levels. As part of advanced remote patient monitoring systems, these tools detect deterioration before symptoms escalate.
Respiratory data is especially valuable in sleep studies, post-op patients, or those on oxygen therapy at home.
What they monitor:
- Breathing rate and volume;
- Nocturnal desaturation or apnea;
- Therapy adherence for nebulizers or CPAP.
Medication adherence tools
These tools ensure that RPM doesn't fail because a patient forgot a dose. Smart pill bottles, dispensers, and even AI-based reminders track usage and send alerts. Integrated into remote patient monitoring technology, they support better chronic condition outcomes and reduce preventable hospital visits.
Caregivers and care teams receive alerts when a dose is missed, helping to close a major gap in real-world patient behavior.
Tool types include:
- Smart caps with light/sound/vibration reminders;
- Mobile apps with refill and timing nudges;
- Connected pill organizers with daily tracking.
Multi-parameter monitoring devices
These all-in-one units simultaneously monitor several metrics – blood pressure, temperature, oxygen saturation, heart rate, and more. Used in hospital-at-home models or high-risk patient programs, these remote health monitoring systems are ideal for scaling care without sending multiple devices.
As mentioned in the Business Wire , these devices reduced hospital admissions by 87% and mortality by 77% in a post-acute RPM setting.
Device features:
- Plug-and-play setup for home patients;
- Unified data feed into one RPM dashboard;
- Reduced equipment load for patients and staff;
These ten devices form the backbone of remote care, from managing diabetes to preventing hospital readmissions. Each plays a distinct role, yet all are part of the same larger shift: moving healthcare from the clinic to the home, powered by real-time data and proactive care.
Whether through a single pulse oximeter or a fully integrated multi-parameter system, remote patient monitoring is becoming the standard of modern, scalable, and human-centered care.
Practical applications of remote patient monitoring
Remote healthcare is now delivered across a wide range of clinical settings. Below are three practical examples of how remote monitoring devices are used in real life.
1. Post-discharge cardiac rehab
After a heart attack or surgery, patients are sent home with a bundle of tools – blood pressure cuffs, ECG patches, and smart scales. These devices help care teams track vitals daily, monitor recovery progress, and intervene early if complications arise. This kind of remote health monitoring has been shown to reduce readmission rates and improve long-term outcomes.
2. Diabetes management in rural areas
Continuous glucose monitors and connected glucometers allow diabetic patients in remote regions to manage their condition without traveling to a clinic. Providers receive automatic updates and can schedule teleconsultations if trends show instability. This is especially critical in underserved communities with limited access to specialists.
3. COPD and respiratory monitoring at home
Patients with chronic respiratory issues use pulse oximeters and smart spirometers to monitor oxygen levels and breathing patterns daily. Combined with wearable alerts, these remote monitoring devices help detect early signs of flare-ups and prevent ER visits, offering both safety and convenience from home.
4. Cancer recovery with temperature tracking
After chemotherapy, cancer patients are especially vulnerable to infection. Smart thermometers are used to track subtle changes in body temperature and flag potential problems early. When integrated with RPM platforms, this monitoring helps detect neutropenic fever, one of the leading causes of hospitalization post-chemo.
5. Postpartum support for high-risk pregnancies
High-risk pregnancies often continue to require close monitoring after delivery. Devices like BP monitors and wearable heart trackers help detect signs of postpartum preeclampsia or hypertension. RPM programs now extend care into the home for new mothers, reducing risk without overloading hospital resources.
Build compliant and secure RPM apps with healthcare software engineering experts
How to choose the right RPM
Choosing the right remote patient monitoring is a meticulous process involving going through many different solutions before determining what's best for your practice.
It's essential to note that for medical monitoring devices to work effectively, they must operate within a unified system. This typically involves the implementation of specific software solutions. Here are some steps that would help you succeed:
- Evaluate the needs of your practice: Before picking the remote monitoring system, you should know for sure what exactly you would like to achieve with it and which data you want monitored. Decide whether it is specific vital signs or issues you must be alerted about.
- Integration with existing systems: Consider how the device you pick interacts with the existing health IT infrastructure and electronic health records (EHR) system.
- Follow centralized data management practices: The software that you pick for remote patient monitoring should be able to receive and store data from various devices in one place.
- Involve user training: All professionals within your hospital or company should be educated on how to use the software and devices and analyze the received data.
Our experience in remote patient monitoring
At Binariks, we help healthcare companies build tailored patient monitoring device solutions aligned with real clinical workflows and regulatory demands. Our team has hands-on experience designing, developing, and scaling connected health platforms supporting real-time tracking and long-term chronic care.
We've worked with clients across the US and EU to build platforms for diabetes management, post-operative care, and cardiovascular health. In one case, we helped a digital health startup launch a custom mobile app integrated with wearable ECG sensors and a cloud-based dashboard for cardiologists.
Another client turned to us to develop a full-stack RPM solution that included data ingestion from Bluetooth home health monitoring devices, integrated alerts, and HIPAA-compliant reporting.
Our teams cover the full product cycle: from UX research and architecture to cloud infrastructure, mobile development, and HL7/FHIR-based integrations. Whether you're building an RPM module from scratch or need to embed monitoring into an existing EHR-connected app, we're ready to support you at any stage.
Let us know what you're building. If your vision includes smarter care through connected monitoring, we'll help turn that into something real and scalable.
Final thoughts
Remote patient monitoring is no longer a niche tool; it's becoming a core layer of modern care. From managing chronic conditions to reducing readmissions and extending care beyond hospital walls, RPM helps healthcare providers stay connected to patients in real time.
But the value isn't just in the data, but in how that data is delivered, interpreted, and acted on. Whether you're building your first RPM platform or expanding an existing solution, choosing the right devices, workflows, and tech partner is key.
If you're exploring custom RPM development or integrating home health monitoring devices into your digital health product, Binariks is ready to help.
FAQ
Share

