Data modernization in healthcare is a strategic issue for healthcare organizations in 2025 and beyond, as companies relying on legacy data systems cannot keep up with their siloed data and extract meaningful insights from it.
This leads to financial losses and kills the quality of care, which is the burden ultimately carried by the patients, and the main reason why having a healthcare data modernization plan is so crucial.
In this article, we share a successful case of a US-based healthcare provider specializing in in-home care. Binariks assisted the company with healthcare data transformation from start to finish, achieving impressive results.
The current state of healthcare data
In most healthcare organizations today, patient information is distributed across a patchwork of legacy electronic health record (EHR) systems. It is very common for various departments to have standalone applications with data that cannot be shared adequately elsewhere due to the creation of data silos. Another problem is that the data is entered manually, which results in bottlenecks.
Another obvious problem is that legacy systems are not built to maintain the scope of data that exists today. The scale of this issue is staggering:
Healthcare already accounts for 30% of the world's total data volume, which is projected to grow at a 36% annual rate over the next several years.
However:
Nearly 80% of healthcare data remains unstructured and underutilized while locked in legacy systems and offline.
This leads to a massive rise in costs and diminished quality of care for patients.
Healthcare data modernization is the only real way to take hold of these issues, and contemporary companies understand that quite well today.
For example, our client, a US-based provider of in-home caregiving services, faced growing operational strain as its patient and caregiver data expanded. As the company grew, the volume and complexity of this data quickly overwhelmed its legacy data infrastructure in healthcare .
Analysts struggled to prepare even basic reports, spending hours manually bringing together inputs from multiple systems. This slowed day-to-day efficiency significantly.
The case represents a clear example of data overload that needs modernisation. Our dedicated IT team at Binariks took on the challenge of solving this issue.
Proven data architecture expertise for enterprise-scale digital transformation and modernization projects
Why healthcare needs data modernization
As medical care becomes more data-driven, the ability to leverage information efficiently is directly tied to caregiver efficiency and, as a result, the quality of patient outcomes.
Data modernization in healthcare is driven by:
- Explosive data growth
- Need for real-time insights
- Regulatory demands
- Need to scale
- Operational bottlenecks
- Need to cut costs and improve regulatory efficiency
Modernization of healthcare data is not just an expensive trend; it helps solve a whole bunch of data-related issues. Our project is again a clear example of that. As our client's patient base and caregiving staff expanded, their analysts struggled with slow dashboards and fragmented data flows.
The resulting bottlenecks directly impacted the quality of their caregiving services, and modernization was the only way to reduce analysts' time to leverage data. To address this, they remodeled legacy data models, modernized the stack, and improved data quality.
This case illustrates that a right healthcare data modernization strategy will help solve administrative issues for healthcare providers. What is more, patients can expect accurate diagnoses and better outcomes.
Ultimately, all stakeholders benefit from healthcare data transformation, even though it could be expensive for companies to create a healthcare data modernization roadmap that works.
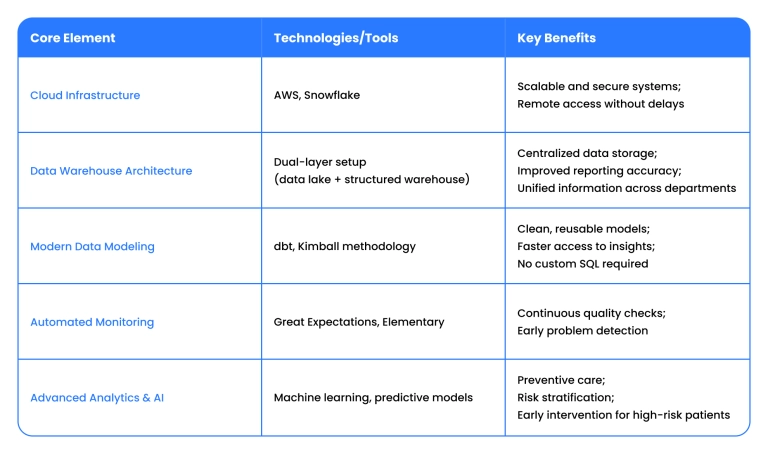
Core elements of healthcare data modernization
Integrating security into data architecture
Modernizing healthcare data infrastructure requires meeting the highest data security standards and regulatory compliance driven by legislation. Below, we break down how secure design is embedded into every layer of data modernization.
Regulatory requirements analysis (HIPAA, GDPR)
Healthcare providers operate under strict regulatory frameworks designed to protect patient privacy and ensure secure handling of sensitive data.
- HIPAA mandates safeguards for Protected Health Information (PHI), including encryption, access controls, and audit trails.
- GDPR applies to organizations handling the data of EU citizens, emphasizing consent, data minimization, and the right to erasure.
- HITRUST & NIST (US): These are supportive pieces of legislation that drive data AI healthcare modernization in the US. They offer actual control frameworks to demonstrate HIPAA compliance. NIST defines technical safeguards(e.g., actual encryption standards); HITRUST integrates HIPAA, NIST, and other standards into a single framework.
- Frameworks such as PIPEDA (Canada) and NHS DSPT (UK) work similarly. PIPEDA aligns with GDPR principles but is less prescriptive. NHS DSPT acts as a healthcare-specific implementation of GDPR requirements in the UK.
Security architecture patterns for compliance
A secure-by-design architecture anticipates threats at every layer. Common patterns used in healthcare data modernization include:
- Zero trust access controls: Access is restricted based on user role, context, and minimum necessary permissions.
- Encryption in transit and at rest: Sensitive data is protected using industry-standard protocols like TLS and AES-256.
- Network segmentation: Tools such as VPCs, IAM roles, and firewalls (e.g., in AWS) isolate critical systems and minimize exposure.
- Auditability and monitoring: Logging, access tracking, and anomaly detection ensure traceability and rapid incident response.
Data classification and handling frameworks
Not all data carries the same level of risk. Implementing a data classification framework allows for differentiated handling based on sensitivity:
- Tier 1: Patient health records (PHI, PII) → strict encryption, restricted access, and full audit logging.
- Tier 2: Operational metadata → encrypted and available to select internal users.
- Tier 3: Anonymized or aggregated data → shared under clear usage terms with minimal sensitivity.
Classification ensures the right controls are applied to the right data.
One of our client's top concerns was ensuring secure collaboration within an outsourced data engineering model. To address this, Binariks proposed several options, including using client-owned devices, virtual machines, and other data-safe deployment strategies.
The client selected a virtualized access environment aligned with their internal compliance policies. This allowed Binariks to confidently embed a senior data engineer into the team while maintaining complete control over data exposure.
Our engineer performed a deep review of the Snowflake- and Tableau-based infrastructure, gathered metadata via APIs, and assessed risks.
Through proof-of-concept validations and stakeholder alignment sessions, Binariks ensured all improvements, from data modelling to monitoring, met both technical goals and regulatory requirements.
Technical steps for secure data processing and storage
A modernized healthcare data stack must be secure by default, as it protects sensitive information during every data lifecycle stage. Here are the key technical practices that enable secure processing and storage:
Encryption strategies for data at rest and in transit
To prevent unauthorized access, encryption must be implemented at two critical stages:
- At rest: All stored data is encrypted using robust standards like AES-256. Services like AWS S3, RDS, and Snowflake support native encryption at rest with managed key or customer-managed key options.
- In transit: All data transferred between systems, services, and users is encrypted using TLS 1.2+ for confidentiality during transmission. This is particularly critical in hybrid cloud and API-based integrations.
In our project, all data layers, whether in the dual storage architecture or analytics tools, were secured with both encryption methods from the start.
Access control and audit logging requirements
Only authorized personnel should access sensitive data; every access must be traceable. Best practices include:
- Role-based access control (RBAC): Access is granted based on user roles, ensuring that every professional only sees the data relevant to their function.
- Multi-factor authentication (MFA): Adds an additional layer of security beyond passwords, often required for administrative roles.
- Audit logging: All access and activity (logins, queries, and schema changes) must be logged and monitored. Logs are centralized and reviewed periodically for anomalies.
In our implementation for an in-home care services provider, we provided clear IAM policies within AWS and enforced strong access logging in Snowflake and other cloud components.
Secure data integration patterns
Connecting internal tools with external (partner systems, third-party services) is risky without the support of a proper structure. Key integration strategies include:
- Token-based authentication (e.g., OAuth2) for secure API access.
- Message queuing and event-driven architecture (e.g., AWS SQS/EventBridge) for asynchronous, decoupled data transfers.
- Isolated VPCs and subnet configurations for partner and external access.
Binariks employed several of these secure patterns while integrating reporting systems for our client's external partners.
Automated compliance monitoring and reporting
Real-time observability tools like Elementary and Great Expectations were used in our project to reduce manual oversight and prepare for audit, in particular:
- Validate incoming data for structure, uniqueness, and completeness.
- Monitor model performance, pipeline durations, and anomaly spikes.
- Send automated alerts via Slack and email when thresholds are breached.
Data governance frameworks and policies
A clear data governance framework defines ownership, access levels, lifecycle rules, and documentation requirements. This includes:
- Data ownership models across departments.
- Data retention policies to comply with HIPAA/GDPR timelines.
- Metadata management to track data lineage and transformations.
Binariks supported the client in establishing internal data ownership protocols around sensitive health and caregiver information.
Incident response and breach prevention
A modernized stack prepared for extraordinary events must include:
- Breach detection systems (e.g., AWS GuardDuty, CloudWatch alerts).
- Response playbooks with containment, investigation, and recovery steps.
- Post-incident audits to identify root causes and improve system resilience.
These practices are integrated into the design at the start so that compliance remains sustainable even as the organization scales.
Successful case studies in healthcare data modernization
Let's again return to a standout example of healthcare data modernization in our practice: the transformation of a New York-based provider of in-home caregiving services.
With over 250 employees and a growing digital platform, the company faced serious challenges of big data in healthcare as its outdated infrastructure struggled to keep pace with real-time operations and scale demands.
As our client's platform expanded through mobile and web applications for caregivers and patients, their internal data systems became a critical bottleneck. Analysts spent excessive time filtering, organizing, and visualizing data, while dashboards lacked consistency and responsiveness. These delays impacted the workflows, as well as the quality and timeliness of care delivery.
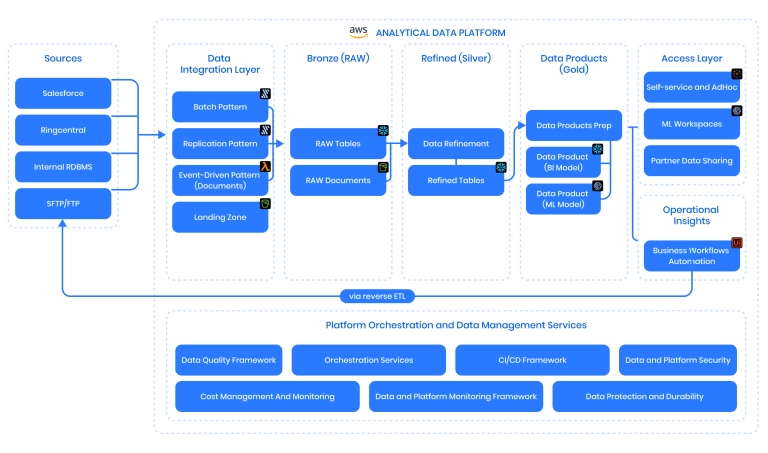
Binariks re-architected the client's data infrastructure from the ground up:
- Implemented a dual-layer architecture with a data lake and warehouse, following Kimball methodology
- Introduced dbt for scalable data modeling
- Deployed Great Expectations for automated data validation
- Integrated Elementary to enable real-time pipeline monitoring and error detection
- Modernized dashboards and introduced role-based access control
- Designed external reporting pipelines for seamless partner collaboration
Key outcomes
- Data ingestion became 50% faster
- Decision-making time was cut by 75%
- Operational costs decreased through automation and streamlined analytics
- Scalability improved, with infrastructure ready to support ongoing growth
- Real-time monitoring allowed for reliability across critical data workflows
- External reporting enhanced coordination with third-party partners
"Automation now gives our team unprecedented clarity into patient data. We can now move faster and smarter without worrying that data will drag us behind." – the client's review
Advantages of modernized healthcare data
Modernizing healthcare data infrastructure reshapes how providers deliver care and, more importantly, how patients receive it. Here is how:
Cost optimization in compliant architectures
Legacy systems come with hidden costs from things like manual reconciliation. In contrast, modern stacks:
- Automate validation and monitoring
- Adopt scalable cloud tools (e.g., Snowflake, ECS) for lower infrastructure and maintenance costs
- Enforce data quality and lineage
These upgrades at our client's company led to reduced overhead, faster reporting, and fewer compliance risks.
Scalable growth in regulated environments
Effective growth requires a flexible and secure infrastructure:
- Dual-layer architectures separate raw from refined data for cleaner analytics
- Granular access control and logging enable secure team expansion
- Reusable data models make it easy to onboard new users, sources, and partners
Our client expanded their caregiver base and external reporting without introducing risk or technical debt.
Other benefits
- Improved clinical decisions via real-time data for accurate diagnosis and early intervention.
- Smarter operations via automation, which streamlines scheduling and claims.
- Better patient experience with faster access to care and improved personalized care.
- Stronger compliance & security through systems built with HIPAA, GDPR, and HITRUST in mind.
- Accelerated innovation thanks to unified data that allows for better clinical research and AI-driven interventions.
- App modernization with support for next-gen applications built around clinician and patient needs.
- Legacy system upgrades and cross-sector collaboration. Outdated siloed systems give way to real-time data sharing and improve coordination between healthcare providers.
- Equity by design: Data modernization strategies that account for underrepresented populations help address disparities and improve access to care.
Challenges of data modernization in healthcare
1. Legacy system integration
Older systems were never designed to support modern analytics, so the integration can be slow even with the best effort, depending on which legacy system is in place.
In the observed case, legacy infrastructure couldn't keep up with growing patient and caregiver needs. Data pipelines were fragmented and brittle.
Solution:
Binariks implemented a dual-layer data lake + warehouse architecture , integrating old sources into a scalable platform without a full system overhaul.
2. Data migration risks
Moving sensitive health data to new platforms is a risk to data integrity. The issues with increased downtime or even data loss are possible.
In our project, analysts needed to migrate live production data while keeping dashboards functional.
Solution:
We used dbt transformations with Great Expectations validation, enabling a phased migration with zero disruption and clean data handoff.
3. Regulatory compliance
Our client required HIPAA compliance while enabling collaboration with third-party teams.
Solution:
We offered secure deployment options, including client-owned virtual machines, and embedded role-based access controls and audit trails to meet HIPAA and NIST.
4. Training & adoption resistance
Teams do not always like new tools, especially if training is lacking, or if they are at a high management level, or at a higher management level, if they don't show value fast.
Analysts were overwhelmed by SQL requests at our client's company, and teams didn't trust outdated dashboards.
Solution:
We introduced dbt-modelled semantic layers and reliable Tableau dashboards, making analytics faster and easier to use without retraining.
5. Disconnected data
Fragmented systems result in duplicated and conflicting information. Much important info goes off record.
At our client's company, patient and operations data were siloed across systems, and everything worked slowly.
Solution:
We unified sources in a central Snowflake warehouse, enabling all teams to access a single source of truth in real time.
6. Talent gaps
There's a global shortage of cloud-native data engineers and healthcare-savvy analysts.
Our client's internal teams lacked deep experience with the tools needed for medical data modernization.
Solution:
We embedded a senior data engineer to lead the Binariks internal delivery team, who worked on the transformation. We also worked closely with analysts and care ops to introduce improvements gradually.
7. High initial costs & ROI pressure
We get it: budget holders want to see business value quickly before investing in a strategy for modernizing healthcare data at scale.
Our client needed visible results before expanding the initiative.
Solution:
We prioritized quick wins (faster dashboards, reduced analyst workload), creating early momentum and justifying further investment.
8. Poor data quality
Inaccurate or inconsistent data undermines all analytics, especially in healthcare. This was a concern in the project we're sharing here.
Solution:
We deployed Elementary and Great Expectations to catch anomalies in real time and flag them to IT.
Conclusion
Data modernization delivers measurable improvements in operational performance and decision-making quality across regulated industries. And the transformation approach demonstrated in our case applies to any organization struggling with legacy systems, fragmented data, and complex compliance requirements.
Here is the healthcare data modernization roadmap for anyone looking to modernize:
1. Assess your current data infrastructure
2. Prioritize business-critical use cases and bottlenecks
3. Improve the factors you are already strong at
4. Choose the right architecture
5. Integrate EHR and non-clinical systems with the right tools
6. Align with real clinical workflows
7. Implement the right governance and monitoring
8. Train and empower your teams
9. Demonstrate ROI and impact early
10. Plan for long-term innovation
Successful data modernization in regulated environments requires deep technical expertise combined with an understanding of compliance frameworks.
Binariks specializes in navigating these complexities – from legacy system integration and secure data pipelines to real-time monitoring and regulatory compliance.
Whether working with healthcare, financial services, insurance, or other regulated sectors, we deliver solutions that transform operations while maintaining the highest security and compliance standards. Our approach ensures organizations can leverage modern data infrastructure to drive better outcomes without compromising on regulatory requirements or data integrity.
Share

