The insurance industry is a complex and highly competitive field that requires efficiency, accuracy, and exceptional customer service to thrive. Central to this industry is claims processing, the procedure by which insurance companies handle claims made by policyholders seeking compensation for losses covered under their policies.
Effective claims processing is crucial for maintaining customer satisfaction and trust, yet it remains one of the most challenging aspects of the insurance business.
Insurance companies face numerous problems in processing claims manually, including:
- Time-consuming procedures: Manual claims processing involves extensive paperwork and verification steps, leading to delays.
- Human error: The reliance on manual data entry and review increases the risk of errors, which can result in incorrect payouts or denied claims.
- High operational costs: Maintaining a large workforce to handle claims can be expensive and inefficient.
Claim processing automation offers a transformative solution to these challenges by leveraging technology to streamline and expedite the entire process. Automation reduces the time required to process claims, minimizes human errors, and significantly cuts operational costs, all while enhancing the overall customer experience.
We at Binariks realize this shift. We focus on the latest tech, guiding insurance companies smoothly from manual to automated systems. Our strength lies in crafting personalized strategies that precisely match each insurance provider's requirements.
In this article, you will gain a comprehensive understanding of:
- Challenges in manual claims automation process and how this automation functions.
- Technologies for automating claims processes and the advantages.
- Selecting claims automation software and popular solutions.
- Integrating automated claims processing systems and implementation costs.
Challenges in manual claims processing
As mentioned, manual insurance claim processing poses significant challenges for insurance companies, impacting operational efficiency and customer satisfaction. Here are the key obstacles:
- High processing time and increased error rates: Manual handling of claims involves extensive paperwork and manual data entry, leading to time-consuming processing cycles and a higher risk of errors such as typos, inaccuracies, and misinterpretations. These delays and inaccuracies can result in prolonged wait times for policyholders and disputes over claim assessments, ultimately affecting customer satisfaction.
- Limited scalability and compliance challenges: Manual processes have limited scalability, making it challenging for insurance companies to efficiently handle claims in high volumes. Scaling manual operations requires significant investment in resources and infrastructure, leading to higher operational costs. Additionally, adhering to regulatory requirements and compliance standards is more complex with manual processes, increasing the risk of penalties and legal issues.
- Poor customer experience: Manual claims processing often results in lengthy wait times, unclear communication, and inconsistent claims handling. This poor customer experience can lead to decreased satisfaction, loss of trust, and negative word-of-mouth publicity, further impacting insurers' reputation and market competitiveness.
- Inefficient resource utilization and data security risks: Manual claims processing can involve repetitive tasks and inefficient resource allocation, leading to suboptimal use of human and financial assets. Moreover, manual handling of sensitive customer data increases the risk of data breaches and compromises data security, posing significant risks to both insurers and policyholders.
- Lack of real-time insights and decision-making: Manual claims processing often lacks real-time visibility into claim status and progress, hindering timely decision-making and proactive management of claims. Without access to accurate and up-to-date information, insurers may struggle to identify emerging trends, assess risk exposure, and make informed decisions, potentially leading to missed opportunities and operational inefficiencies.
By automating claims processing, insurers can tackle these challenges head-on, leading to smoother operations, happier customers, and a competitive edge in the market.
How claims process automation works
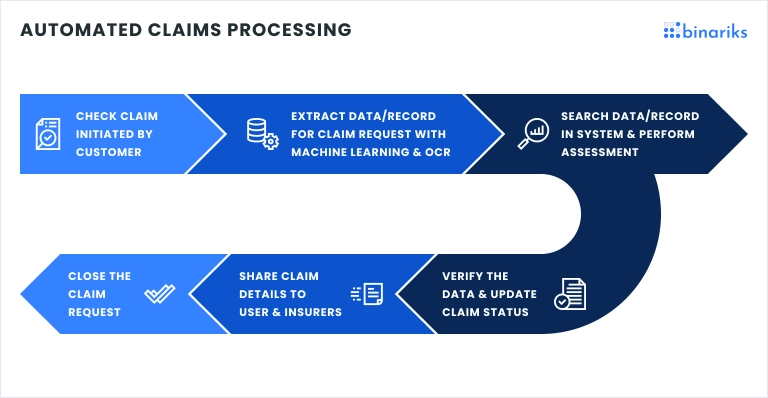
Claims automation in insurance involves using advanced technologies such as artificial intelligence, machine learning, and robotic process automation to streamline and optimize the entire claims' lifecycle. Automation solutions are designed to handle various tasks, including:
- Data capture and extraction: Automated systems capture and extract relevant data from multiple sources, including claim forms, documents, and digital channels.
- Claims validation and adjudication: AI-driven algorithms assess claim validity, verify policy coverage, and determine claim eligibility, reducing the need for manual intervention.
- Fraud detection and risk assessment: Machine learning models analyze claim patterns and historical data to detect anomalies, flag potential fraudulent activities, and assess risk levels.
- Claims settlement and payment processing: Automated workflows facilitate seamless claim processing, from adjudication to settlement and payment disbursal, ensuring timely and accurate compensation for policyholders.
- Communication and customer interaction: Chatbots and virtual assistants provide real-time support to policyholders, addressing queries, providing status updates, and guiding them through the claims process with minimal human intervention.
Technologies used in claims processing automation
Modern technologies are critical to claim management automation, as they are for the insurance industry in general. In this section, we examine what is driving automation efforts and changing the way claims are handled.

Artificial intelligence
AI technologies, including intelligent document management, form the backbone of any claims processing automation system. These technologies enable enhanced decision-making and predictive analytics by analyzing vast data sets to detect patterns, trends, and anomalies. This integration boosts claims assessment accuracy and fraud detection efficiency.
For instance, NLP aids in automated information retrieval and sentiment analysis from unstructured text data, while OCR helps extract data from scanned or image-based PDFs. Intelligent document management streamlines data interpretation and processing, leading to remarkable time and cost savings.
Check out our AI Claims Processing Guide to learn more about the role of AI in claims management.
Natural language processing
NLP technologies enable automated extraction and interpretation of unstructured text data from documents, emails, and customer interactions. NLP algorithms analyze language patterns, extract relevant information, and categorize data for efficient claims processing.
By understanding and interpreting human language, NLP enhances the accuracy of information retrieval, claims assessment, and customer communication, thereby improving overall efficiency and satisfaction.
Machine learning
ML algorithms empower claims automation systems to learn from historical data, enabling personalized risk assessment, claims triaging, and settlement optimization.
ML models continuously evolve and adapt to changing claim patterns, providing insurers with actionable insights for process optimization and decision support. Predictive modeling techniques within ML forecast claim volumes, assess risk probabilities and optimize claims processing workflows for better resource allocation.
Robotic process automation
RPA bots automate repetitive, rule-based tasks in claims processing, such as data entry, document processing, and claims validation. RPA enhances operational efficiency by reducing manual effort and increasing processing speed, leading to claim adjudication and settlement faster.
Also, RPA bots integrate seamlessly with existing systems, allowing insurers to achieve significant cost savings and productivity gains across their claims operations.
Data analytics and predictive modeling
Advanced data analytics techniques and predictive modeling tools leverage historical claims data to forecast claim volumes, assess risk probabilities, and optimize claims processing workflows.
Data analytics platforms provide insurers with actionable insights into claim patterns, fraud detection trends, and customer behavior, enabling proactive risk management and strategic decision-making. Predictive modeling capabilities within analytics solutions empower insurers to anticipate claim trends, identify emerging risks, and allocate resources effectively to optimize claims processing efficiency.
Adopting these technologies in claims process automation represents a paradigm shift in the insurance industry.
Benefits of automating claims processing
By automating insurance claims processing, companies can significantly improve their operations and deliver superior service to their policyholders. Here is a list of benefits and some interesting examples.
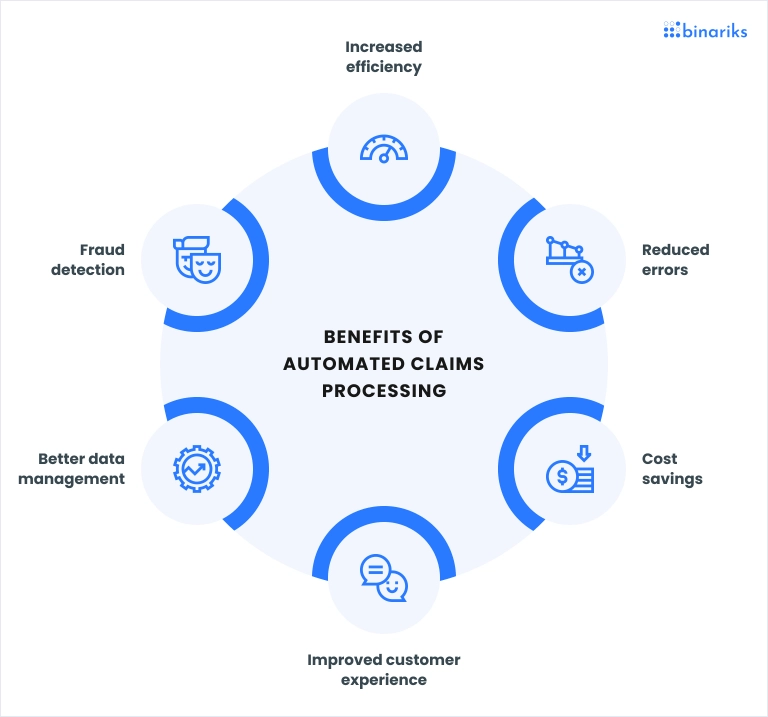
- Increased efficiency and speed: Automated claims processing reduces the time required to handle claims by streamlining workflows and eliminating manual tasks. This leads to quicker settlements and improved customer satisfaction.
- Enhanced accuracy and reduced errors: Automation minimizes human errors by using AI and machine learning for data extraction and analysis. This ensures more accurate claim assessments and fewer disputes.
- Cost savings: Automated claims processing leads to substantial cost savings by reducing manual labor and processing times. It also helps identify and prevent fraudulent claims, reducing associated costs.
- Improved customer experience: Faster and more accurate claims processing results in shorter wait times and more transparent communication. Automated systems provide real-time updates and instant support, enhancing customer satisfaction.
- Better compliance and risk management: Automated claims processing ensures adherence to regulatory requirements and compliance standards. Advanced analytics and predictive modeling help insurers manage risks more effectively.
- Employee satisfaction: By freeing employees from manual claims processing, they can focus on value-adding activities such as handling complex claims, brainstorming new products, and providing better customer service .
What to look for in claims process automation software
To automate claims processing, it is essential to select a solution that encompasses a comprehensive suite of features tailored to the insurance industry's specific requirements. Here are the critical considerations to bear in mind when choosing your automation software:
Integration capabilities
The software should seamlessly integrate with your existing systems, such as CRM, ERP, and other core insurance platforms. This ensures smooth data flow and reduces the need for manual data entry, enhancing overall efficiency.
Advanced data analytics
Look for software that offers robust data analytics and reporting tools. Advanced analytics can provide valuable insights into claim trends, detect fraud, and improve decision-making processes.
AI and machine learning
AI and machine learning capabilities are essential for automating complex tasks like data extraction, claim assessment, and fraud detection. These technologies enhance accuracy and speed up processing times.
Scalability
Choose software that can scale with your business. As your company grows, the software should be able to handle increasing volumes of claims without compromising performance.
User-friendly interface
A user-friendly interface is critical for ensuring your team can easily adopt and use the software. Intuitive design and easy navigation reduce training time and improve productivity.
Compliance and security
The software should comply with industry regulations and standards, ensuring all claims data is handled securely and confidentially. Look for features like encryption, audit trails, and regular compliance updates.
Customizability
It is essential to be able to customize the software to meet your specific needs. Look for solutions with configurable workflows, rules, and templates to fit your unique processes.
Some popular claims automation software
Selecting the appropriate claim management automation solutions that align with your specific needs is vital. Here are five solutions specifically designed for the insurance industry.
1. Guidewire ClaimCenter
Guidewire ClaimCenter is a comprehensive claims management system tailored for the insurance sector. It provides end-to-end claims processing solutions that streamline workflows and enhance operational efficiency.
Key features:
- End-to-end claims management from FNOL (First Notice of Loss) to resolution
- Integrated analytics and reporting tools
- Flexible architecture, supporting custom workflows and integration with other systems
2. Duck Creek Claims
Duck Creek Claims offers a robust platform for managing the entire claims lifecycle. It is designed to help insurers handle claims more efficiently, from initial report to settlement, leveraging advanced analytics and automation.
Key features:
- Comprehensive claims management capabilities
- Advanced analytics for improved decision-making
- Scalable platform supporting integration with various insurance systems
3. Insurity Claims Decisions
Insurity Claims Decisions is a cloud-based solution that enhances claims processing through automation and data-driven insights. It helps insurers reduce processing times and improve accuracy.
Key features:
- Cloud-based platform for flexibility and scalability
- Automation of routine tasks to reduce manual effort
- Data analytics for better insights and fraud detection
4. Snapsheet Claims
Snapsheet Claims focuses on digitalizing and automating the claims process. It offers mobile-friendly solutions that improve customer interactions and streamline the workflow for insurers.
Key features:
- A mobile-friendly platform for enhanced customer engagement
- Automation of claims workflows to improve efficiency
- Integration with existing systems for seamless operations
5. FINEOS Claims
FINEOS Claims is a core system designed for large insurance carriers. It offers comprehensive claims management capabilities and automates the claims process to improve service delivery and operational efficiency.
Key features:
- Comprehensive claims management for large carriers.
- Automation and workflow management tools.
- Advanced analytics for operational insights and fraud prevention.
Embrace InsurTech innovation with custom software development
Integrations for automated claims processing systems
Integrating claims processing automation software with existing systems is a critical step for insurance companies aiming to streamline operations and maximize the benefits of automation. Effective integration ensures seamless data flow, enhances functionality and improves overall efficiency.
Core insurance systems
Integration with core insurance systems, such as policy administration, underwriting, and customer relationship management (CRM) systems, is essential.
This connectivity allows for real-time data exchange and ensures that all aspects of the insurance lifecycle are aligned. For instance, claims data can be cross-referenced with policy details to verify coverage quickly, reducing the time required for claim approval.
Document management systems
Claims processing automation often involves handling a significant volume of documents, such as bills, receipts, and medical reports. Integration with document management systems enables automated data extraction and categorization, facilitating quicker and more accurate claims processing.
This setup also supports digital storage and retrieval, reducing the reliance on paper documents and enhancing data security.
Fraud detection systems
Integrating fraud detection systems with claims automation software enhances the ability to identify and flag potentially fraudulent claims.
Advanced analytics and AI can be employed to analyze patterns and anomalies in claims data, helping insurers mitigate risks and reduce losses due to fraud. This integration allows for proactive measures and faster resolution of legitimate claims.
Customer communication platforms
Effective claims management requires timely communication with policyholders. Integrating customer communication platforms, such as email, SMS, and chatbots, with claims automation software ensures that policyholders receive real-time updates on their claims status.
This integration enhances customer satisfaction by keeping them informed and engaged throughout the claims process.
Analytics and reporting tools
Integrating advanced analytics and reporting tools with claims processing automation gives insurers valuable insights into claims trends, processing times, and operational performance.
These tools enable data-driven decision-making, helping insurers optimize their processes and improve overall efficiency. Comprehensive reports and dashboards clearly show key metrics and performance indicators.
Implementation costs
When considering the cost of claims processing automation, several key features significantly impact the overall expense:
- User roles and permissions (40-80 hours): Implementing different user roles and permissions, such as adjusters, supervisors, and administrators, requires additional development effort to ensure secure access and data protection.
- Integration with third-party systems (80-200 hours): Integrating the claims processing automation system with external systems, such as payment gateways, document management systems, and regulatory compliance tools, adds complexity and cost to the development process.
- Customizable workflows (80-160 hours): Designing customizable workflows tailored to the insurer's specific processes and requirements involves extensive customization and development work, contributing to higher development costs.
- Reporting and analytics (60-120 hours): Incorporating robust reporting and analytics features to track key metrics, generate insights, and identify trends requires advanced development and data visualization capabilities, increasing the overall cost.
- Mobile accessibility (80-160 hours): Ensuring mobile accessibility for claims processing and allowing adjusters to access the system anywhere require additional development effort to create responsive and user-friendly mobile interfaces.
Development process
- Requirements analysis (40-80 hours): Conducting thorough requirements gathering and analysis to understand the insurer's specific needs, workflows, and regulatory requirements.
- Design and prototyping (40-80 hours): Creating wireframes and prototypes to visualize the system's user interface, functionality, and workflow, ensuring alignment with the insurer's expectations.
- Development (400-800 hours): Developing the core features and functionality of the claims management system, including user authentication, claims processing workflows, integration with third-party systems, and reporting tools.
- Testing and quality assurance (160-320 hours): Performing rigorous testing to identify and fix any bugs or issues, ensuring the system's stability, reliability, and security.
- Deployment and maintenance (40-80 hours): Deploying the claims management system to production environments and providing ongoing maintenance and support to address any post-deployment issues, updates, or enhancements.
The cost of developing an insurance claims management system can vary widely, generally ranging from $50,000 to over $500,000. These figures reflect industry averages, taking into account the specific features required, the complexity of integration, and scalability needs.
However, every insurance company has unique operational requirements and budget considerations. At Binariks, we craft customized solutions tailored to your needs. For a precise estimate that aligns with your requirements, don't hesitate to contact us for a detailed consultation.
Insurtech Application
We built a scalable, user-friendly frontend and refactored the platform code.
Conclusion
At Binariks, we are well aware of the complexities and nuances of insurance claims automation. Our software development and implementation expertise allows us to tailor solutions to your needs and requirements. Whether you're seeking to integrate third-party systems, customize workflows, or enhance reporting capabilities, our team is dedicated to delivering innovative solutions that drive efficiency and maximize your return on investment.
Don't let manual claims processing hold your business back. Contact us today to learn more about how we can support your automation initiatives.
Share

