The role of AI in claims processing deserves separate attention within the framework of analyzing the impact of AI on the insurance industry as a whole. This is because claims processing has its own set of specific challenges and requirements. When it comes down to it, claims processing is a critical touchpoint in the customer's journey with an insurance company.
This article will highlight how AI works for claims insurance, the benefits of claims automation with AI, the use cases of AI claims, and their limitations.
Key aspects described in this article are:
- Claims processing in insurance: The end-to-end process of evaluating claims made by policyholders. It's central to customer trust and operational efficiency.
- How AI works in claims: AI tools like chatbots, OCR document extractors, and fraud detection models support and automate key steps, from intake and validation to decision-making and escalation.
- Benefits of using AI: AI speeds up decisions, lowers operational costs, reduces errors, and helps detect fraud while improving the experience for both customers and adjusters.
- Real-world use cases: Insurers apply AI for damage estimation, fraud flagging, subrogation alerts, and automated payout processing.
- Limitations of AI in claims: AI is not infallible, and human oversight is crucial, especially in complex cases. Legal, ethical, and regulatory concerns must also be addressed.
Benefits of AI for claims processing
There are many benefits to claims automation with AI, but they all lead to the same result – faster solutions, reduced costs and workload, and better customer satisfaction . All of this creates a competitive advantage for an insurance company that uses AI-based claims management automation.
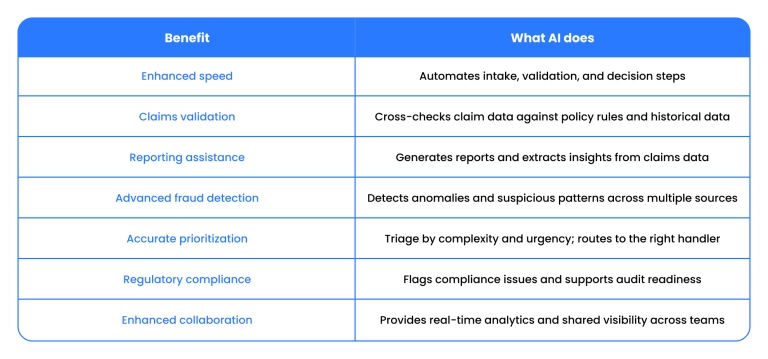
Enhanced speed
Traditional claims processing methods are time-consuming and involve manual data entry and analysis. AI algorithms can quickly analyze vast amounts of data, reducing the time required to process a claim.
AI claims processing means quicker resolution, reduced costs, and better customer satisfaction. Claims processing using AI helps to automate up to half of all claims workflow. A recent study suggests that automated AI systems have cut claims processing time by up to 70% compared to manual processes, while also delivering fraud detection accuracy above 95%.
Claims validation
AI systems are adept at validating claims by cross-referencing data against predefined criteria and historical data.
They can automatically verify the accuracy of claims data, identify inconsistencies, and ensure that each claim complies with policy terms. This reduces human error and provides a more accurate validation process. The result, again, is saved costs for everyone involved.
Reporting assistance
AI can assist in generating detailed and accurate reports. It can analyze data and provide insights that would be time-consuming to extract manually. These reports can be used for internal auditing and compliance, as well as to improve decision-making processes.
AI-driven analytics can identify trends and patterns in claims data. The result is better strategic planning and resource allocation.
Advanced fraud detection
AI algorithms are particularly effective in detecting fraudulent activities in claims. They can analyze patterns and anomalies that might indicate fraudulent behavior. They have helped insurers reduce fraud-related activities by about 40% and improve the detection of subtle patterns that traditional systems miss.
When detecting fraud, AI in insurance claims uses information from various sources. Sources can be external, not just the claimant's information and historical data.
Automated claims management can learn from past fraud cases and adapt to recognize new types of fraud, becoming more efficient over time. This not only saves costs associated with fraudulent claims but also helps maintain the integrity of the claims process.
Accurate prioritization
AI claims solutions can help prioritize claims based on their complexity and urgency. As a result, more critical or time-sensitive claims are handled first by more highly skilled professionals adept at particular tasks.
Moreover, AI can assess and categorize claims based on various factors, enabling claims handlers to focus their efforts where they are most needed. In the end, productivity increases while the workload decreases, and everyone is satisfied.
Regulatory compliance
AI can help ensure that claims are processed in compliance with regulatory requirements. It can automatically check for compliance and flag any issues. Companies using AI claims management have a reduced risk of regulatory fines and reputational damage. Real-time analytics can also help prioritize claims more effectively by assessing risk and urgency.
This is especially important for heavily regulated industries like insurance and surveillance companies with AI capabilities, so it is beneficial for insurance companies to keep up.
Enhanced collaboration between teams
AI insurance claims tools can improve collaboration among teams and departments by providing real-time data and instant access to analytics. This facilitates better coordination and decision-making across the entire organization.
This is crucial for the decentralized workforce of today, where most professionals work remotely, as face-to-face collaboration between departments is often a thing of the past.
Modernize insurance. Lead with innovation
Explore how to overcome the most pressing industry challenges with advanced technology – starting now

Limitations of AI claims automation
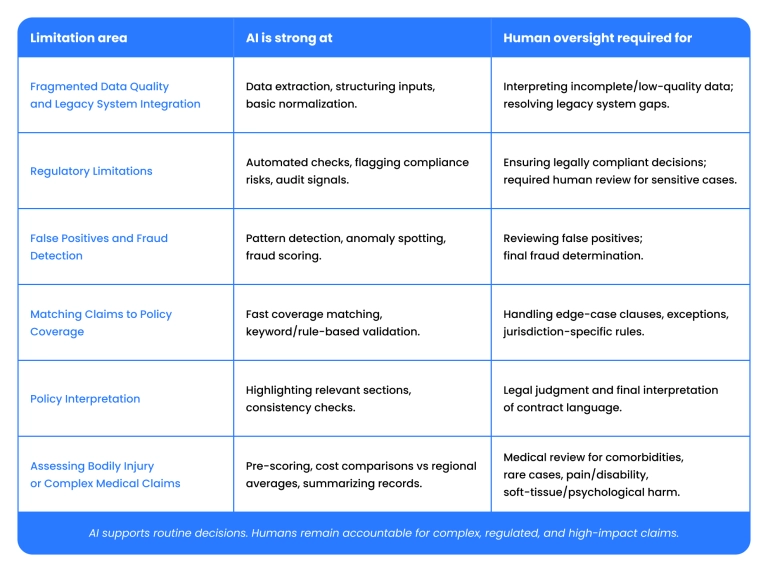
Fragmented data quality and legacy system integration
The data in insurance may not be of high quality or sufficiently consistent for accurate predictions. It is common for insurers to have high-quality auto insurance data, but still store health data in old PDFs. Moreover, many insurers still run on legacy policy and claims platforms that were not designed for AI integration.
Regulatory limitations
Insurance is a heavily regulated industry. In the US, AI in claims management must comply with privacy and data-use laws, such as HIPAA, anti‑discrimination laws, and insurance-specific regulations.
Not everything goes smoothly when using AI to cover these kinds of tasks. In health insurance, US lawsuits have alleged that automated systems helped drive claim denials (which regulators say must include human review).
False positives and fraud detection
AI can detect patterns suggestive of fraud more quickly than humans. Still, it also produces false positives, which are legitimate claims flagged for investigation, especially when unusual but valid circumstances appear. Manual reviews are required to address false-positive claims.
Matching claims to policy coverage
AI is used to automatically validate whether a claim falls under covered conditions based on policy language, but this validation is not always correct. Insurance policies contain edge-case clauses, exceptions, and jurisdiction-specific rules. All of these have to be validated by humans.
Policy interpretation
Insurance contracts are legal documents. Regulators generally hold that only a human, usually an experienced adjuster or medical reviewer, can interpret and apply policy language to an individual claim in a legally adequate way. Automated systems can assist but not replace that legal judgment.
Assessing bodily injury or complex medical claims
AI models are being used to pre-score injury severity or compare treatment cost estimates with typical regional averages. However, current models cannot reliably account for many relevant factors, including chronic conditions, comorbidities, or subjective factors like pain and long-term disability.
Even injuries themselves are not always ideal subjects for AI-driven claims processing. For example, claims involving soft-tissue injuries (e.g., whiplash) or psychological harm still require medical review, and AI often underestimates them.
When AI in claims automation is necessary
If you are in the insurance business, without a doubt, you need AI in claims processing automation.
AI claims processing helps with so many things, including:
- Handling a high volume of claims
- Faster processing times
- Fraud detection
- Cost reduction
- Data-driven insights
- Customer experience improvement
There is no better thing for automated and routine tasks than AI claims management, given its precise ability to analyze large amounts of data. However, there are many instances where it is best not to use AI and rely on humans only, as AI has limitations where human expertise and empathy should come forward.
AI in insurance claims is inappropriate for complex decision-making requiring human judgment to end experience. Consider a healthcare claim involving a patient with a rare, multifaceted medical condition. Let's say the treatment plan proposed is experimental and not widely recognized.
In this case, AI might struggle to accurately assess this claim due to the rarity and complexity of the case. It requires medical expertise and the judgment of actual human professionals to understand the condition's nuances and the plans for the upcoming treatment.
AI also has nothing on humans in situations requiring empathy for human suffering. In fact, we would go as far as to say it is deeply unethical and inhumane to rely on AI claims solutions in sensitive situations. After a catastrophic event like a major hurricane, many homeowners file insurance claims for property damage, and insurance agents should show understanding of the trauma the customers experience.
Finally, claims processing automation is not a solid choice where biased or incomplete data is involved. It takes human experts to recognize data bias. For example, An AI system used in auto insurance claims processing might be trained on data that reflects historical biases, such as higher claim denial rates in a particular area.
If the AI continues to be trained on this data without correction, it could perpetuate these biases, leading to a disproportionate number of claim denials in this area.
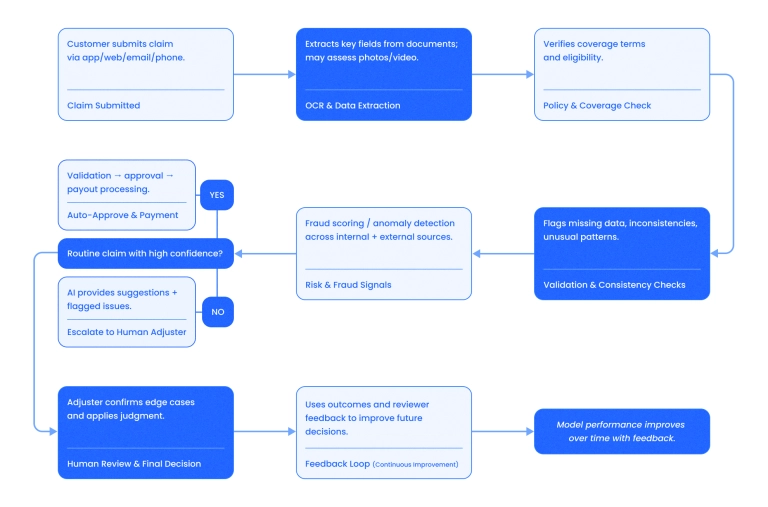
How does it work?
So, how does processing AI claims actually work?
Artificial intelligence claims processing works by analyzing incoming claims data, verifying it against the policy, and either resolving the claim automatically or forwarding it to a human adjuster if an automatic resolution is not possible. AI-driven claims processing is integrated with the insurer’s internal systems, customer-facing apps, and third-party data sources.
When a claim is submitted, AI extracts key information from documents using OCR, checks coverage terms, and may assess photos or video of the damage.
For routine claims, it can handle everything end-to-end, including validation, approval, and payment. In more complex cases, AI doesn't make the final decision. It flags inconsistencies, makes suggestions, and forwards them to a human adjuster for a final decision.
The system continuously improves over time, using feedback from both customers and human reviewers to learn which decisions worked well and which resulted in errors.
Let's look into the process step-by-step in more detail:
5 Сlaims processing automation examples
1. Automating claims intake
A global corporate investigations firm addressed Binariks to streamline the claims intake process for their Australia-based operations team.
They needed artificial intelligence in claims processing to address 2–3-hour delays caused by manual data entry from emails into TrackOps. The company had 20–30 unstructured document layouts, leading to many transcription errors and bottlenecks.
Binariks implemented an AI-driven pipeline using Amazon Textract + Claude Sonnet for document parsing, with a fallback UI for low-confidence cases.
As a result, the client achieved:
- Turnaround reduced to under 15 minutes (from 2–3 hours)
- Manual effort cut by 80–90%
- Parsing accuracy reached 85–90%
- Infrastructure costs are kept under $2,000/year
2. Modernizing FNOL and post-claim systems
A major global Property and Casualty insurer (50,000 employees, $45–50B revenue) partnered with Binariks' tech team to enhance its digital First Notice of Loss (FNOL) and post-claim systems. The main goal was optimizing FNOL workflows .
FNOL data from multiple channels wasn't integrating efficiently with the CMS, which resulted in delays and expensive downtime. We applied a middleware system enabling real-time integration between FNOL inputs and the CMS, and introduced backend services for claim registration.
The results included:
- Reduced manual claim handling and downtime
- Improved system stability
- CI/CD migration and structured QA enabled faster development cycles
3. AI-powered risk evaluation for commercial claims processing
A global commercial insurer replaced its manual document-review workflow with an AI system to process thousands of claims daily. Claims and risk analysts relied on SharePoint to manually extract insights from unstructured insurance documents, a process that was inconsistent and difficult to audit.
Binariks implemented an AI pipeline combining OCR, RAG (LangChain + LangGraph), citation-backed LLMs, and reflection agents within the constraints of Azure.
The key outcomes included:
- Successful implementation of claims automation for risk management
- 90% reduction in time spent on risk data extraction
- 80–90% fewer manual reviews, due to citation-traceable insights
- 20–30% improvement in LLM output quality and confidence
- Reduced compliance risk and improved SLA adherence
- Infrastructure ready for 5x scalability using modular microservices
4. Predictive analytics tool in auto claims
Predictive analytics can forecast the likelihood of claims based on customer profiles and historical data. It is used heavily for risk assessment and fraud detection.
Aviva Canada integrated a real-time predictive analytics tool into its ClaimCenter system to support the auto claim setup process. The Vehicle Remedy Tool instantly analyses incoming claim data and returns accurate repair predictions in approximately 5 seconds.
This replaced a slower, manual setup workflow and helped significantly reduce customer cycle times.
5. AI chatbot automating insurance payouts
US-based car insurer Metromile implemented AVA, a conversational AI assistant designed to streamline claims processing.
AVA interacts directly with policyholders, verifies claim legitimacy using internal rules and AI models, and pays out in straightforward cases without human involvement. According to the company, AVA handles 70–80% of claims immediately, significantly reducing time to resolution and easing adjuster workload.
Take your software to new heights with AI/ML solutions
The future and forecasts
After analyzing many aspects of AI-driven claims management, we can confidently predict how these technologies will evolve.
Integrated IoT and AI for real-time processing
Many insurers already use telematics and connected device data (especially in auto insurance) to speed up claims insights. Telematics data are increasingly fed into AI models to help reconstruct incidents and accelerate first notice of loss (FNOL). While full real-time automated claims initiation is not yet widespread, pilot programs and partnerships between insurers and telematics providers are growing.
In the future, in the event of an accident, vehicle sensors would be analyzed by AI in real time to assess damage, determine fault, and begin claims automatically.
Advanced predictive analytics for personalized insurance
Many insurers today use predictive analytics to segment risk and set premiums more precisely than traditional actuarial approaches in AI-driven claims analysis . They combine internal claims history with external data (e.g., weather, demographics). However, fully personalized pricing based on behavior, lifestyle data, or multi-source feeds such as social media is still emerging and is often limited by privacy and regulatory considerations.
In the future, AI will use data from various sources, including social media, IoT devices, and past claims, to create highly personalized insurance profiles. Insurers will offer dynamic pricing models and personalized coverage options based on individual risk assessments.
Enhanced fraud detection using deep learning
Fraud detection powered by machine learning and deep learning is already in production at many large insurers that invest in AI/ML development .
These detection systems go beyond rule-based checks by analyzing complex, non-linear patterns across historical claims, behavioral data, provider networks, and transaction metadata. They are actively used to flag both known fraud typologies and previously unseen patterns.
The use of deep learning for automated claims processing will become more sophisticated in the future. The models are increasingly being extended to cross-dataset and cross-domain analysis, combining claims data with external sources (public records, network graphs, unstructured text, images, and sometimes near-real-time signals).
Voice-activated virtual assistants for claim management
Chatbots and virtual assistants are widely used for basic customer interactions (e.g., reporting a claim, checking status), but most are script-based and limited in complexity.
Right now, voice-activated AI that can understand nuanced natural language and handle complete claims workflows is in pilot or limited release.
By 2028, over 60% of insurance customer interactions are expected to be handled by conversational AI or voice assistants, particularly in claims intake and status tracking.
AI-driven predictive claims routing
Some insurers use automated routing based on simple rules (e.g., injury claims go to a medical specialist team). More advanced predictive routing with AI recommending the best agent is in early adoption stages. Vendors are introducing intelligent route optimization into modern claims platforms.
In the future, AI will automatically route claims to the most appropriate handler, improving turnaround time and service quality.
Blockchain and AI integration for transparency and efficiency
The use of blockchain in insurance is expected to grow at a CAGR of over 55% through 2030, with claims processing as the primary use case. In the future, insurers would use blockchain as an external verification layer for claims data, with AI monitoring integrity and exceptions across parties.
Self-learning AI systems for continuous improvement
AI systems will continually learn from each claim processed, becoming more efficient and accurate.
These self-learning systems could adapt to new claims and evolving regulatory landscapes without explicit reprogramming. They will become more accurate with less retraining.
Use of AR and VR for claims assessment
Insurers might use augmented reality (AR) and virtual reality (VR) technologies powered by AI to assess claims. Some insurers already use AR tools for remote visual inspections to support adjusters; for example, customers can upload photos or use AR overlays to document damage.
VR applications are less common and are mainly used for training rather than for live claims. Adoption is increasing as device costs fall and visual AI improves. Remote AI-assisted visual inspections can reduce on-site assessment costs by up to 40% and shorten settlement timelines by several days.
Emotion AI for enhanced customer interactions
Emotion AI (systems that infer sentiment from voice, text, or facial cues) is currently used primarily in contact centers to score customer mood for quality monitoring or agent support.
Few insurers use it directly in claims interactions, but vendors are beginning to offer emotion-aware modules that can tailor responses for empathy. In the future, AI systems will respond not only with accurate information but also adapt their tone and communication to emotional context.
Embrace InsurTech innovation with custom software development
Final thoughts
To conclude, in the 2020s, an insurance company has every reason to use AI for automated claims management. It saves costs, improves customer satisfaction, enhances reputation, and is a win for everyone involved.
One important thing to do is to be aware of AI limitations in insurance. Even though insurance claims processing requires AI, experienced human professionals remain as important as ever, especially when dealing with complex claims and regulatory limitations.
If you are going to develop a claims processing automation solution today, the cost can be as low as $6,000 for a basic AI chatbot for first notice of loss (FNOL) and policyholder interaction, to between $50,000 and $100,000 more for complex AI solutions, like fraud detection software.
A team of professional AI developers at Binariks can assist you with all your AI claims management software needs.
FAQ
Share

